Ankle surgery.
Haglund’s Deformity
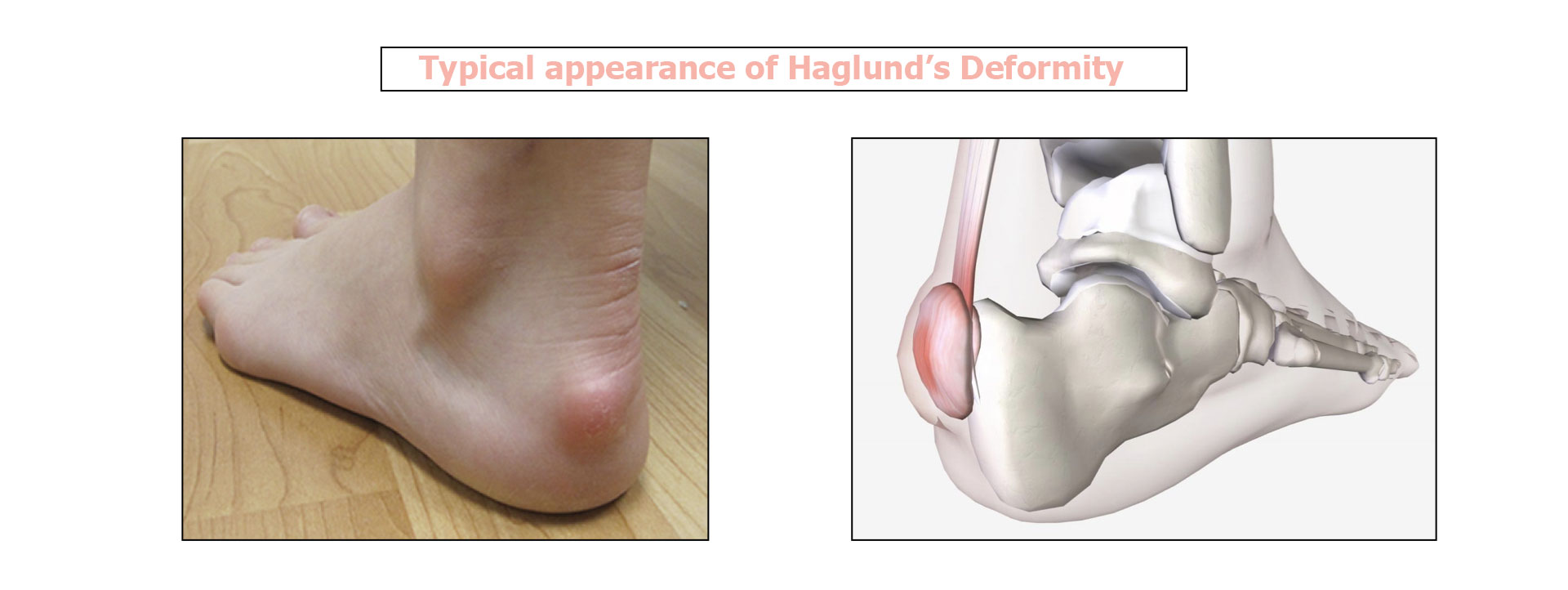
A Haglund’s Deformity happens when the Achilles tendon becomes irritated at the point where it attaches to the calcaneus (heel bone). It results in a bony enlargement at the back of the foot, causing sharp pain in the heel. The enlargement gradually leads to retrocalcaneal bursitis, which can become very painful. The area rubs on the stiff back of shoes, creating pressure and irritating that part of the heel. It should initially be given medical treatment, but if that fails then surgery is an option.
Contents
- Video presentation
- What is Haglund’s Deformity ?
- What is the treatment for Haglund’s Deformity?
- Preparing for surgery
- Hospital stay & procedure
- After the surgery
- Recovery period & Return to work
- Potential complications
Haglund’s Deformity is a type of Achilles tendon enthesopathy, which affects the attachment of the Achilles tendon to the calcaneus (heel bone).
The deformity was first described in 1927 by a Swedish surgeon called Patrick Haglund. It causes a bump and pain at the back of the heel where the Achilles tendon attaches to the bone.
Initially the condition was thought only to affect women who wore high heels. However, various studies now show that anyone can suffer from a Haglund’s deformity, and that shoes are not the main cause.
What are the risk factors for Haglund’s Deformity?
- A naturally prominent heel bone on the outer side of the foot, making the heel more likely to rub against the back of shoes
- Walking with the weight on the outside edge of the foot, known as supination
- A short Achilles tendon, which can place added pressure on the heel bone
- A hollow foot, causing the heel to tilt slightly when walking and the Achilles tendon to rub against shoes
A Haglund’s deformity can be caused by wearing certain types of shoes. Some shoes can make the condition worse and trigger severe pain, making it hard to wear shoes at all.
Shoes and boots with a stiff upper can also cause rubbing that aggravates a Haglund’s deformity.
People with these types of feet should avoid wearing stiff shoes and make sure all footwear is well-fitting.
What types of shoes are most often linked to Haglund’s deformity?
- Ice skates and roller skates
- Dress shoes, including for men, and stilettos
- Steel-toe work boots
- Stiff winter boots or rain boots
What are the symptoms of Haglund’s Deformity?
- Pain at the back of the heel when walking and doing sport
- Pain when pressing the bump
- Visible bump at the back of the heel
- Swelling or redness of the heel
- Corns or blisters on the heel where the bump rubs the shoes
The diagnosis is based on clinical signs i.e. the existence of the deformity and the associated pain.
Additional tests are then required to determine the type of treatment.
What additional tests are needed?
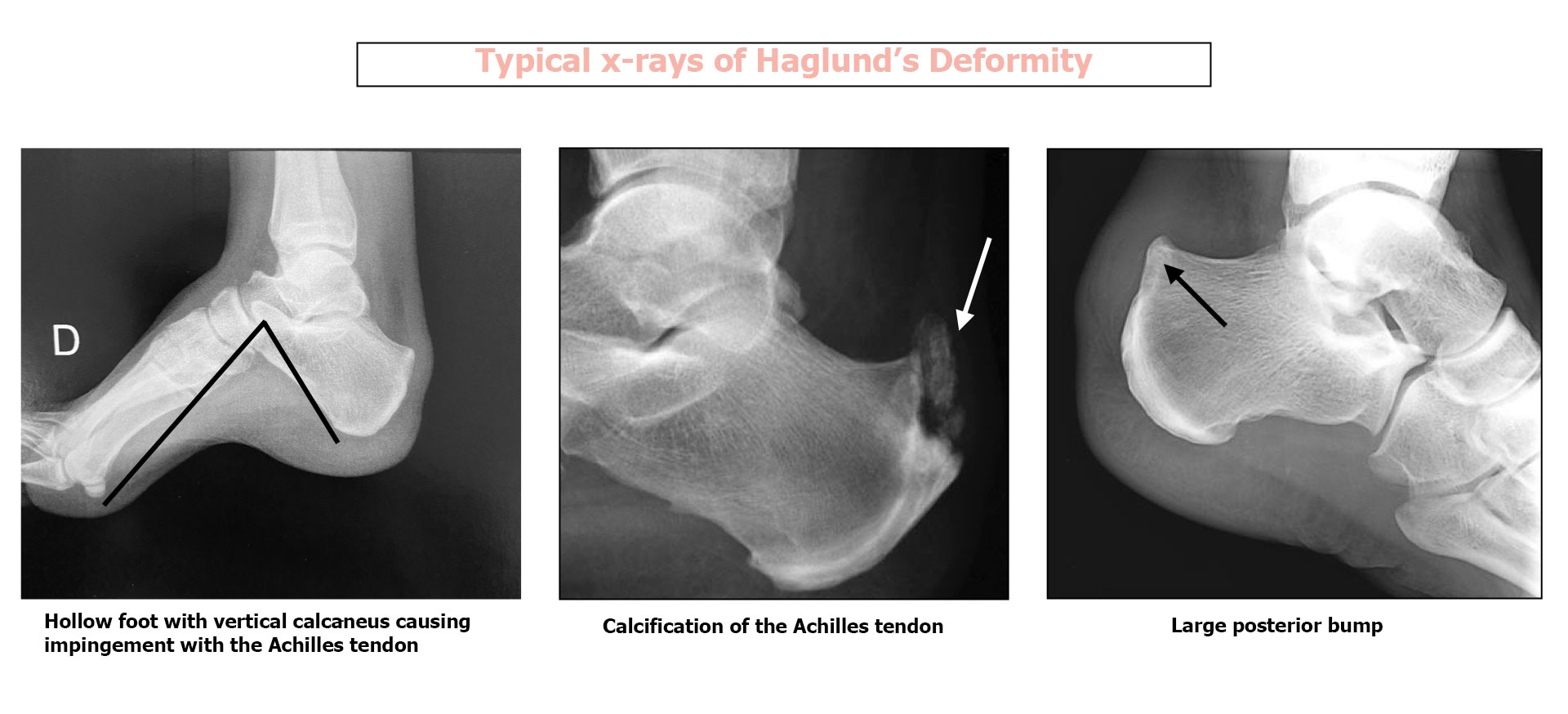
1 Lateral x-ray of the ankle :
The radiographer will look for various signs:
- General shape of the heel bone and extent of the posterior deformity
- Calcification where the Achilles tendon attaches to the heel bone
- Shape of the foot (hollow or flat) For a severely hollow foot (vertical calcaneus) the treatment will be different.
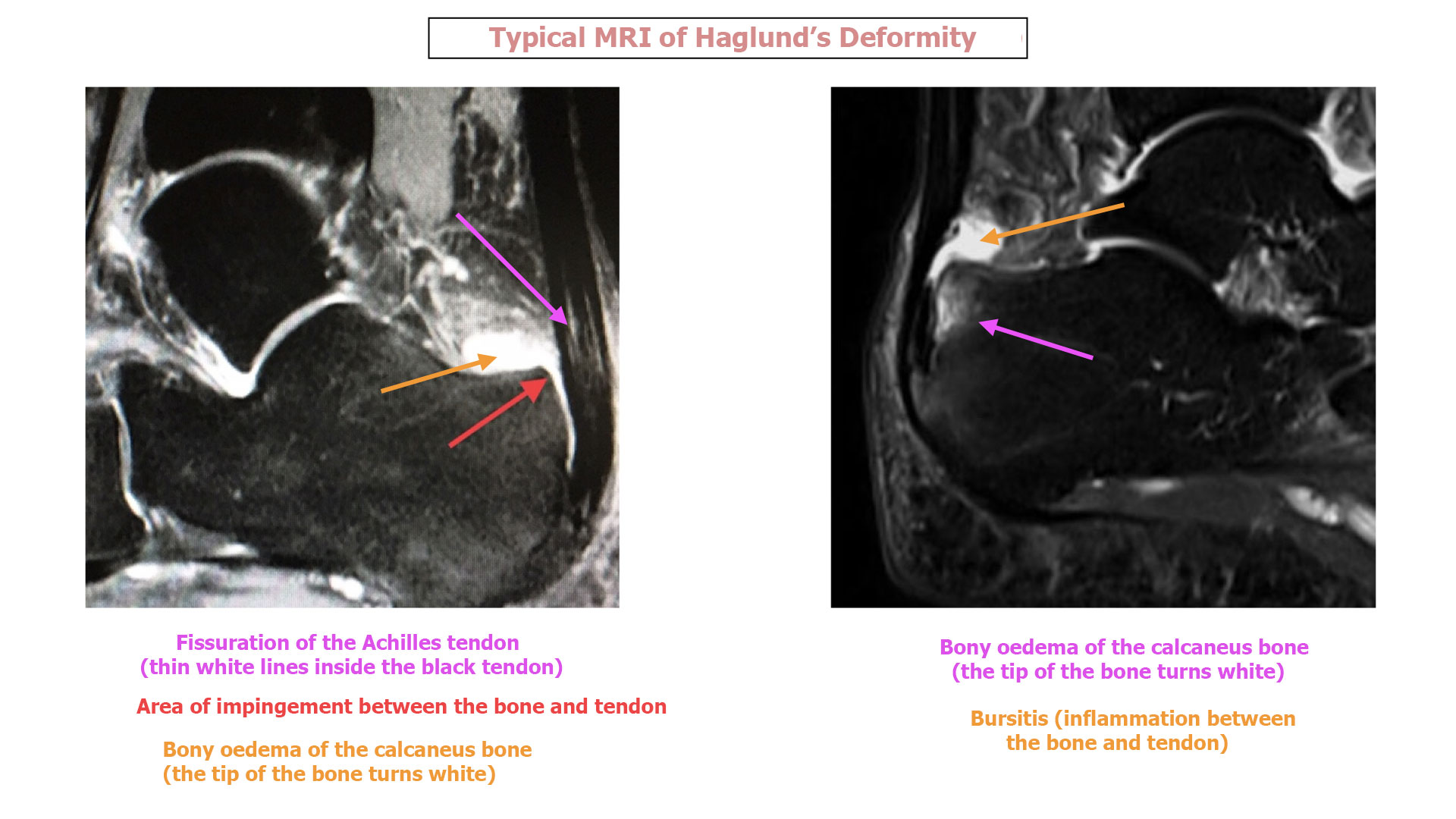
2 MRI of the ankle :
The MRI will look for various signs:
- Hyperintensity in the posterior calcaneus, indicating inflammation of the bone where it attaches to the Achilles tendon
- Bursitis (inflammation of the bursa) in front of the Achilles tendon
- Tendinitis (inflammation and fissuration) of the Achilles tendon. Any tendinitis will then require combined treatment of the bone and tendon.
NON-SURGICAL TREATMENT :
Medical treatment should always be tried first, in order to avoid surgery if possible. The following options are available:
-
-
- Medication: anti-inflammatory drugs to help reduce the inflammation. The treatment may comprise pills or a topical cream for the painful area.
- Cryotherapy: an ice pack is placed on the painful area (with a thin cloth between the ice and the skin) for 20 minutes first thing in the morning.
- Exercises: Achilles tendon stretches to reduce the tension on the calcaneus. These exercises are especially good for people with a short Achilles tendon.
- Heel pad: use an orthopaedic insole with a heel pad to raise the bone and stop the Achilles tendon pulling on the calcaneus.
- Different shoes: wearing shoes with a flat sole or a soft upper can avoid or minimise the irritation.
- Physiotherapy: Some types of physiotherapy, such as ultrasound therapy, can sometimes reduce the inflammation.
- Immobilisation: in certain cases, you may have to wear a cast to reduce the symptoms (this is rarely used in practice and is very restrictive).
- Injections: Steroid injections into the bursa can help the diagnosis and treatment. (Injecting steroids directly into the Achilles tendon is not recommended because it can weaken the tendon and cause it to tear).
-
SURGERY :
If medical treatment is not enough to relieve the pain, you may be offered surgery.
Surgery involves removing the inflamed bursa or sac, along with the bony enlargement. The procedure can be performed using either a traditional open technique, which leaves a 1.5–2” scar (4–5cm), or a minimally-invasive endoscopic technique that requires just two tiny incisions. Your doctor can discuss the potential side effects of each type of surgery and what is best for you.
For some patients, an endoscopic calcaneoplasty (removing part of the heel bone using minimally-invasive surgery) can be a good choice for treating a Haglund’s deformity. It has fewer complications after the surgery, allows you to put weight on the foot sooner after the procedure, and can involve a shorter recovery time and less time spent with the condition.
A suitable preoperative consultation is needed to make sure the surgery is the right choice for you. It may involve the injection of a local anaesthetic directly into the bursa between the bone and the tendon. If the pain then disappears for a few hours, this confirms that the problem is in fact a Haglund’s deformity and not another condition and will give an idea of whether an endoscopic calcaneoplasty will work.