Hip Surgery
Total Hip Replacement
Osteoarthritis of the hip is a degenerative condition that affects the hip joint. It causes increasing degrees of hip pain, which gradually reduces the distance a person can walk. It becomes harder to move the hip, causing sufferers to lose their independence. There are many treatments to slow down this condition (e.g. injections, viscosupplementation). A total hip replacement is the last resort and involves surgery to replace the joint with a prosthetic hip in order to alleviate the pain and restore the patient’s independence.
Contents
- File information
- Description & progression
- Diagnostic & indication chirurgicale
- Preparing for surgery
- Hospital stay & procedure
- After the surgery & results
- Recovery period & Return to work
- Potential complications
Osteoarthritis of the hip happens when the surfaces inside the hip joint become worn and the cartilage gradually disappears. This wearing away gets worse over time, causing abnormal friction, pain and stiffness in the joint (limited flexion and internal rotation). The wearing away of the cartilage is irreversible and there is no cure for osteoarthritis. The only thing you can do is slow it down.
Some of the clinical signs can be very disabling for day-to-day life:
- Reduced walking distance
- Difficulties with stairs, especially when coming down
- Difficulties cutting your toenails, and putting on socks and shoes
- Difficulties getting up from an armchair or low seat
- Pain at night
Osteoarthritis is a degenerative condition which means it is linked to wear and tear, but there are also extrinsic factors that can accelerate the progression of the disease. The main causes are:
- Hip surgery, especially during childhood (e.g. epiphysiolysis)
- Fractures (e.g. femoral head, acetabulum) or a history of hip dislocation
- A rheumatic disorder (e.g. chondrocalcinosis, synovial chondromatosis, rheumatoid arthritis)
- Malalignment of the femoral neck (coxa vara, coxa valga)
The first step in treating osteoarthritis is to give medical treatment i.e. pain relief. This is often combined with hygiene and dietary measure to alleviate the pain. Patients are often advised to lose weight and do regular exercise (such as walking, swimming, cycling or general physical therapy to increase muscle strength). Injections of hyaluronic acid and cortisone are also required to lubricate the joint and protect the damaged cartilage.
If medical treatment is no longer having the desired effect, the only way to relieve the pain is with surgery.
This means a total hip replacement.
The diagnosis is based on the clinical history, with patients often clearly describing pain for many years, a gradual reduction in the distance they are able to walk, initially when going up or down stairs and when walking on uneven ground, and eventually when walking on flat ground.
X-rays are essential for confirming the diagnosis, including frontal images of the pelvis and frontal and side images of the damaged hip. The images will reveal joint impingement (a narrowing of the distance between the joint surfaces) indicating loss of the cartilage. No other examinations are necessary, unless there is any doubt over the early-onset osteoarthritis or suspected necrosis. In this case, an MRI may be requested.
A Total Hip Replacement is indicated when medical treatment no longer has any effect. The procedure offers functional treatment with the sole aim of improving the patient’s quality of life. It is therefore ultimately up to the patient to decide whether to go ahead with the operation. Dr Lévy will try to explain what will happen in either scenario, with and without the surgery. The operation is recommended for patients whose daily lives are being affected by disabling pain in the knee. This disability should be significant, and not just occasional. There is no hard and fast rule, because every patient is different. There is no age limit for a total hip replacement, but it should be avoided in young patients because the only limitation of the procedure is the life span of the implants which will eventually have to be replaced if the patient is too young; although sometimes, there is obviously no other option. Fortunately, there have been great improvements in implant quality and they now have a much longer life span.
Ultimately, the need for surgery will be decided after a long discussion between the patient and surgeon.
SURGICAL CONSULTATION:
The aim of the preoperative consultation with the surgeon is to establish a diagnosis. Dr Lévy will examine the hip to determine how much the joint is damaged. He will analyse the patient’s gait (to check for any limp) and determine whether there is any pain when flexing or internally rotating the hip. He will check to see whether there is any difference in leg length that can be corrected during the operation and look for any vascular problems in the legs by feeling for the pulses.
X-rays and other test results will be used to help plan the surgery. Depending on the damage and its cause, Dr Lévy will decide what is required. He will explain what will happen during and after the surgery, as well as any potential complications. This will include a discussion of how long the treatment will last, the recovery time and any rehabilitation required after the operation.
You will be given time to discuss your options, and you will receive advice on the pros and cons of the surgery.
Once a decision has been made, Dr Lévy will take some blood and urine samples in order to make sure you have no infections. He will also ask for an x-ray of your teeth to rule out a dental infection. You will have to see a cardiologist and get their go-ahead for the surgery. Finally, you will have an appointment with the anaesthetist.
ANAESTHETIC CONSULTATION:
Once the indications have been confirmed, one of Dr Lévy’s assistants will give you an appointment with the anaesthetist who will look after you during the operation. The anaesthetist will examine you and prescribe any additional tests that may be needed before the surgery. He or she will also explain how the anaesthesia works and the best method for you. The procedure is usually carried out under general anaesthesia.
SMOKING :
It is essential to stop smoking one month before and after the surgery. This is because a mass influx of nicotine reduces blood flow and slows down the healing process. You may use extended-release nicotine patches to help with the withdrawal symptoms.
You will stay in hospital for about a week. This time will be used to treat the initial pain, monitor the wound and start your rehabilitation.
The procedure is usually performed under general anaesthesia. It takes about 60–90 minutes. Dr Lévy uses the posterior minimally-invasive approach, meaning the cuts he makes through the muscles are as small as possible in order to avoid destabilising the joint and minimise the pain after the operation. The piriformis muscle does not get cut, which improves implant stability after the operation. The benefit of this technique over the anterior approach is greater accuracy when restoring leg length. In addition, there is no risk of damage to the nerves which can sometimes happen with the anterior approach (meralgia paresthetica, also known as lateral femoral cutaneous nerve entrapment). The risk of dislocation is very slightly higher than with the anterior approach, but the difference is negligible when using a minimally-invasive technique that spares the piriformis muscle. Dr Lévy will select the size of the implant in advance using the x-rays and templates for each of the various components. He can then select the perfect size implant for each patient. Ultra-precision instruments are used to place the implant as accurately as possible, based on the advance planning, in order to ensure the joint is as stable as possible and both legs are the same length.
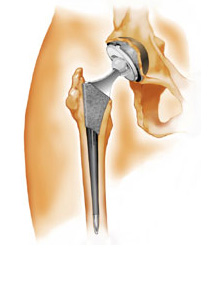
There are four parts to the implant:
- A femoral component made from chrome/cobalt, which gets fixed to the femur (the femoral stem)
- A ball made of alumina ceramic (the femoral head)
- A component made from chrome/cobalt, which gets impacted into the pelvis (the metal-backed acetabular cup)
- An insert made of alumina ceramic, which gets inserted inside the metal-backed cup (the acetabular insert)
Dr Lévy will carefully secure haemostasis (cauterise the blood vessels) to keep the blood loss to a minimum. A process called autologous blood transfusion is often used – the blood shed during the surgery is centrifuged, concentrated, then reinfused back into the patient to avoid the need for a subsequent blood transfusion. Autologous transfusions are safe because they use the patient’s own blood. There is therefore no risk of contamination or rejection.
Once the operation is finished, you will be transferred to the recovery room where your vital signs and pain levels will be monitored. Any autologous transfusion will take place in the recovery room. You will spend about two hours there.
Then you will return to your room to rest. The next day, the nurses will administer any painkillers prescribed by the anaesthetist, and you will receive a visit from the physiotherapist to start your rehabilitation. You will receive a private physiotherapy session every day. For some of the first day, you will be allowed to sit up in a chair.
You will usually be able to try standing on the second day; after that you can take a few steps, first with a walker then with two crutches. The physiotherapist will first focus on daily activities (e.g. standing up, walking, sitting down, lying down).
As you improve, you will attempt walking up and down stairs.
Patients are usually discharged to their home, but will continue to receive daily visits from nurses, assistants and physiotherapists under the PRADO home care protocol.
During the first month you will be allowed to walk as much as you like without limits. Physical therapy/rehabilitation will start as soon as possible, focusing first on actions that will allow the patient to regain their independence. The nursing team will also give you injections of anticoagulants (for 30 days) and change your dressings. You should do your exercises every day to help your hip recover as much mobility as possible. The skin staples will be removed between day 15 and 21.
POSTOPERATIVE CHECK-UPS :
30-DAY CHECK-UP :
Until this appointment you will have to wear compression stockings (which will have been prescribed in advance) and you should have already begun physiotherapy to restore joint range. The swelling in the leg knee will have begun to go down a little bit, and it will be less painful. Dr Lévy will examine the scar, your mobility, and determine whether there is any residual pain. He will look at your new x-rays and make any necessary adjustments to your recovery plan for the next few months. You will be able to drive again after 30 days. Until the next check-up you will not be allowed to sit in a low chair and must use a toilet seat elevator to avoid dislocating the implant.
4-MONTH CHECK-UP :
Physiotherapy will now focus on strengthening the gluteus muscles to stabilise the hip. You should begin to forget all about your prosthetic hip. Your muscles may not quite have regained full strength, and you can improve it with either exercises at home or physiotherapy. Dr Lévy will give you advice to avoid damaging the implant.
If your hip is stable and the gluteus muscles nicely toned, he will allow you to resume cycling and swimming.
12-MONTH CHECK-UP :
It is important to have an annual check-up of the implant. By now you should have long-forgotten the joint and been able to resume normal life and sports (e.g. golf, tennis, skiing).
RESULTS :
Hip replacement surgery gives excellent results. A total hip replacement will give you a completely normal hip i.e. you will forget all about it over time.
The average life span of a total knee replacement is now 20–25 years. After this time it will need to be replaced. The second operation is often more complicated than the first time, and the results not quite as good.
You should see your surgeon for a check-up every year, with x-rays to check for any complications. This will just be a short appointment so he can check the scar, your movement, any pain and take some x-rays.
You must take every precaution against infections and treat any infection as quickly as possible (dental, sinus, urinary infections etc.). This is because the bacteria could migrate to the shoulder at any time and infect the implant, in which case the only option will be to have it replaced.
You will be able to walk again immediately after hip replacement surgery.
You can resume driving after 30 days.
The amount of time you need to take off work will depend on your job.
For office workers, this may be a matter of days.
For physical jobs or jobs where you need to stand all day, the average time off work is six weeks.
However, you may need to spend even longer off work if your job is incompatible with your recovery.
A wide range of complications can occur with surgery. Fortunately, they are very rare and the various appointments before and after the surgery are designed to avoid them or detect them early if they do appear.
As well as the risks common to all types of surgery and the risks of the anaesthesia, there are some specific risks associated with this procedure.
The following complications may occur with hip replacement surgery:
SURGICAL SITE HAEMATOMA :
A haematoma is a rare but serious complication. It happens when there is bleeding from a small vessel in the hip, filling the space with blood. The thigh swells and becomes painful and taut. If it gets too swollen, the surgeon may have to perform further surgery to locate the leaking blood vessel and cauterise it.
SURGICAL WOUND INFECTION :
Despite all the precautions taken by the operating team, bacteria may still enter the wound either during the surgery or afterwards, before it is fully healed. This compromises the healing (more redness around the wound than normal), causing severe pain, a purulent discharge and a persistent fever.
You must tell the surgeon if you see any of these signs and seek EMERGENCY treatment.
DO NOT TAKE ANY ANTIBIOTICS BEFORE SEEING THE SURGEON.
Dr Lévy will decide whether to wash out the hip and send any samples for testing, in order to prescribe the correct antibiotic for any infection, assuming it has been caught in time. Otherwise, the implant will have to be replaced. This is a major operation to treat the infection and can mean the functional results are not as good as was originally expected. You will also have to take antibiotics for at least 45 days and have regular check-ups with the surgeon. It is a serious complication.
IMPLANT DISLOCATION :
This is a rare but very annoying complication. When it happens, it does so within the first few months after the operation. It can be caused by an inadvertent movement (a fall, sitting too low down with the leg rotated internally during the first few months). The two halves of the implant – the head and the acetabulum, get separated. It is very painful and you will have to be sedated for a brief moment to put the implant back in place.
PHLEBITIS/PULMONARY EMBOLISM :
Despite the preventive anticoagulant treatment given after the surgery and despite wearing compression stockings, a clot may still form in the leg veins (phlebitis) and require long-term curative anticoagulant therapy.
JOINT STIFFNESS :
This can be a knock-on effect of inflammation (algodystrophy) and requires targeted physiotherapy. If you have not regained your full range of motion after three months, it could be caused by fibrosis which requires surgery.
COMPLEX REGIONAL PAIN SYNDROME :
Complex Regional Pain Syndrome, also called algoneurodystrophy, is a condition involving pain and other unpleasant symptoms in a joint after surgery or a fracture. The syndrome may have a neurological cause such as damage to the peripheral nervous system, affecting either the small fibres which protect from pain or heat stimuli, and/or the large fibres which detect tactile stimuli. It causes pain and severe stiffness that can last for up to 18 months. Patients always recover fully. Dr Lévy will diagnose the condition using scintigraphy (a scan) and will support you throughout, in order to treat the painful and unpleasant symptoms.
IMPLANT LOOSENING :
This is not a complication but a natural problem as the implant gets older. After several years, the implant can become loose and cause pain. It will need to be replaced. An undetected infection could cause an implant to loosen sooner than expected. This is known as septic loosening. The surgeon will always check for an infection in case of early loosening.
NERVE DAMAGE :
A very rare complication when the sciatic nerve gets pulled and damaged. The sciatic nerve sometimes runs very closely alongside the pelvis and has to be moved aside by the surgeon when cutting into the joint. Occasionally, this can cause paralysis or paresis (weakness) of the muscles used to raise the foot. Fortunately, this problem is usually only temporary and goes away in a few months.
DIFFERENCE IN LEG LENGTH :
One of the key aims of the operation is to make both legs the same length. In very rare cases, the surgeon discovers that only way to make them the same length would be by making the implant less stable. In this case, it may be necessary to make the operated leg a few millimetres longer in order to avoid dislocation. This difference will never be more than 1cm and is usually unnoticeable in day-to-day life. If it causes problems, the patient can wear an insole for the other leg.
This list does not cover all the possible risks.
Ask Dr Lévy if you want more information, especially if you have any questions about your particular situation and the advantages, disadvantages and risk/benefit ratio of each procedure.