Knee surgery
Meniscus tear
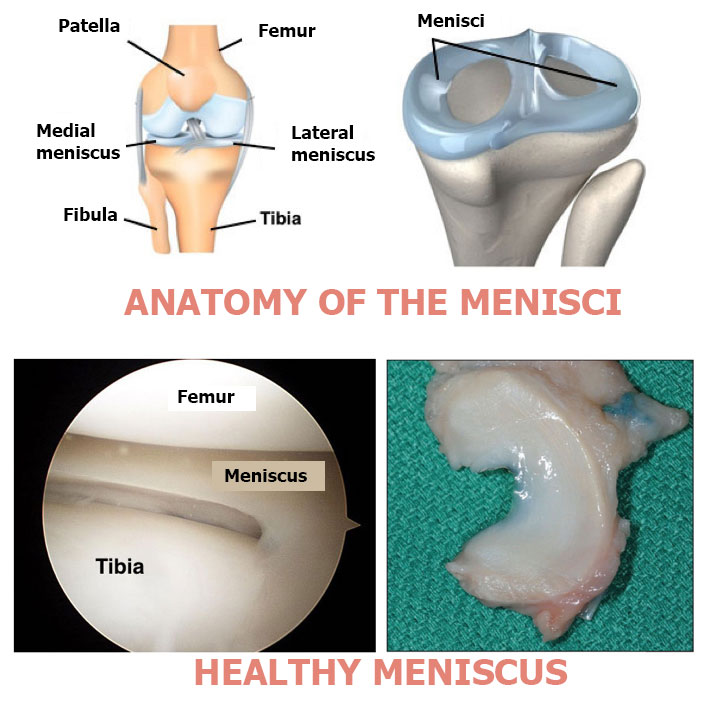
The meniscus is a piece of fibrous cartilage that sits between the shin bone and the thigh bone. There are two in each knee, a lateral meniscus and a medial meniscus. Meniscus injuries are very common and may be degenerative (wear and tear) or traumatic. They are usually treated with arthroscopic surgery. The operation involves either a meniscectomy (removing the damaged piece of meniscus) or a suture (to repair the tear).
Contents
- Video Presentation
- Description & progression
- Surgical indication
- Preparing for surgery
- Hospital stay & procedure
- After the surgery
- Recovery period & Return to work
- Potential complications
Each knee has two menisci, a lateral meniscus and a medial meniscus. The meniscus is a piece of fibrocartilage located between the shin bone and the thigh bone. It stabilises the knee and acts as a shock absorber between the femur and tibia.
Meniscus injuries are tears caused by trauma or gradual wear. They can be painful. They must be treated by an orthopaedic surgeon, although surgery is not always necessary.
DEGENERATIVE MENISCUS INJURIES :
This type of meniscus injury is caused by wear and tear and does not involve any trauma. The pain appears gradually and is mainly on the inside of the knee. It usually happens in cycles of greater and lesser pain. These injuries may occur alongside osteoarthritis of the knee and cartilage damage. The treatment for degenerative injuries is much less surgical than for traumatic injuries
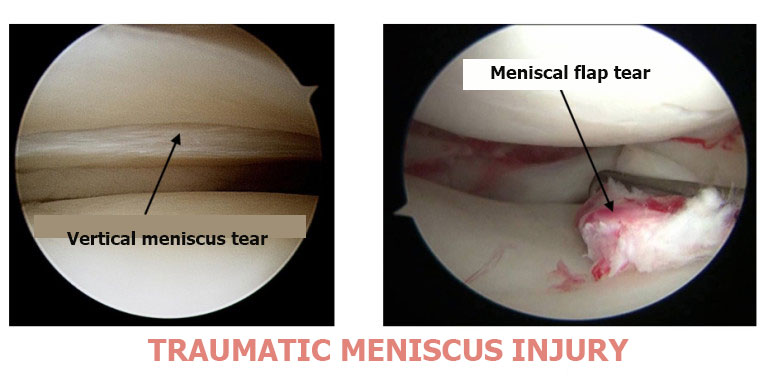
TRAUMATIC MENISCUS INJURIES :
This type of injury may occur alongside anterior cruciate ligament damage or a sprained knee. Twists and sprains often damage the meniscus. The damage may happen at the same time as an anterior cruciate ligament tear or be secondary to a tear. Other mechanisms may be involved, such as suddenly standing up from a crouched position. The patient often hears an audible snap and the knee locks in flexion. This may indicate locking of the knee due to a bucket handle tear. The meniscus tears and flips over itself inside the knee joint, stopping the knee from extending. Traumatic lesions usually require surgery.
MAIN SYMPTOMS :
Pain: usually on the inside of the leg (medial meniscus is most commonly affected) when flexing.
Hydrarthrosis: swelling due to repeated effusion of synovial fluid into the joint.
Clicking: due to a meniscal flap tear.
Locking: due to a bucket handle tear (meniscus flips over and locks the joint).
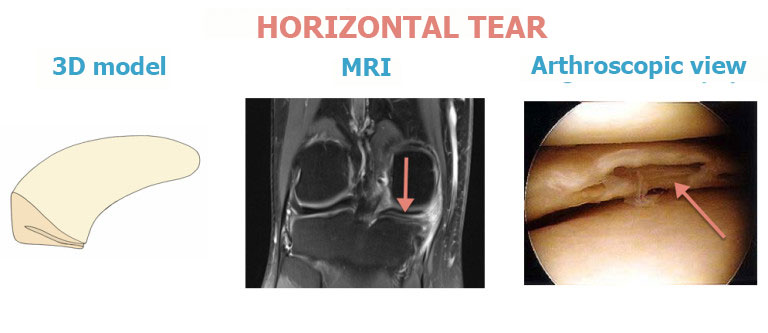
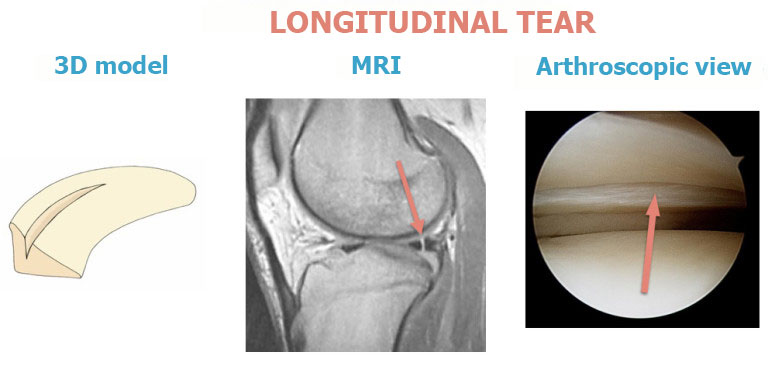
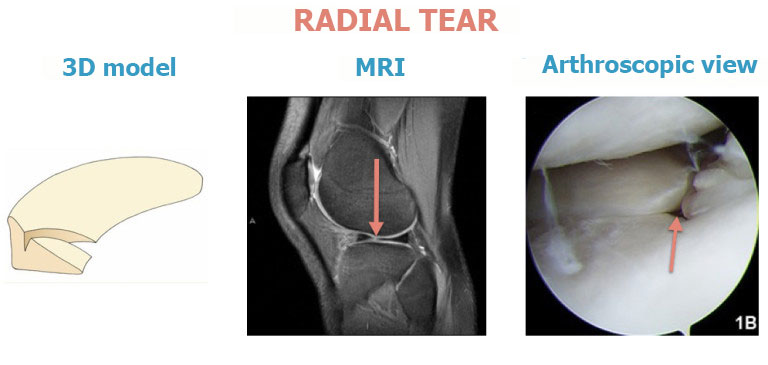
The injuries can be diagnosed with an MRI which is the main diagnostic test.
DEGENERATIVE MENISCUS TEARS :
The first approach is medical treatment. Steroid injections will be given to reduce the inflammation around the damaged meniscus and alleviate the pain.
If medical treatment fails, surgery will be used to remove the damaged meniscus in a procedure known as a meniscectomy.
TRAUMATIC MENISCUS INJURIES :
Traumatic lesions usually require surgery. This type of procedure is routinely performed as part of a ligamentoplasty for a torn anterior cruciate ligament. Depending on the type of damage, the age of the injury and the age of the patient, the meniscus can either be repaired (suture repair) or removed (meniscectomy).
LOCKED KNEE :
In some cases the knee can lock out and no longer be straightened. This happens when part of the meniscus moves out of place, known as a bucket handle tear. It requires emergency surgery to unlock the knee. During the operation and depending on the type of damage, the surgeon will either suture the tear or perform a partial meniscectomy.
SURGICAL CONSULTATION:
The aim of the preoperative consultation with the surgeon is to establish a diagnosis and analyse the pain and loss of function. Dr Lévy surgeon will examine the knee to check whether the pain is consistent with the injuries seen on the MRI. In some cases, the MRI may show meniscus injuries but there is no pain when palpating over the menisci. In this case, the surgery should be cancelled and other causes investigated. He will check whether there are any contraindications to the surgery, such as poor skin or vascular condition or even a hyperintensity on the MRI in the tibial bone beneath the meniscus, which could suggest progressive osteoarthritis that could sharply deteriorate after a meniscectomy.
X-rays and an MRI will be used to help plan the surgery. Depending on the damage and its cause, Dr Lévy will decide what is required. He will explain what will happen during and after the surgery, as well as any potential complications. You will be told whether you will have a meniscectomy or a suture repair.
ANAESTHETIC CONSULTATION:
Once the indications have been confirmed, one of Dr Lévy’s assistants will give you an appointment with the anaesthetist who will look after you during the surgery. The anaesthetist will examine you and prescribe any additional tests that may be needed before the surgery. He or she will also explain how the anaesthesia works and the best method for you.
SMOKING :
It is essential to stop smoking one month before and after the surgery. This is because a mass influx of nicotine reduces blood flow and slows down the healing process, especially following a suture repair. You may use extended-release nicotine patches to help with the withdrawal symptoms.
The surgery is usually carried out as an outpatient procedure (day hospital). Spinal anaesthesia (an epidural injection in the back to numb both legs) is the most common. The surgeon will look inside the knee using arthroscope, a small video camera inserted through a 1cm incision in the knee. Using a second incision the same size, the surgeon will then insert instruments to repair or remove the meniscus.
MENISCECTOMY :
The aim of the surgery is to remove the damaged part of the meniscus, leaving the rest intact. Dr Lévy will attempt to spare as much of the meniscus as possible. In fact, the more that gets removed, the faster the knee will degenerate after the surgery. During the procedure, he will assess the entire joint, looking at the condition of the cartilage in every compartment of the knee, the condition of the cruciate ligaments and the other meniscus.
MENISCUS SUTURE REPAIR :
The aim of the surgery is to repair the damaged part of the meniscus. This type of repair is only possible for certain cases (e.g. young patient, recent injury, good vascularisation). The tear is sutured using arthroscopic suture techniques. This involves mini anchors attached either side of the tear. The anchors are joined with sutures; when the surgeon pulls on the suture thread it then closes the tear. The knee must then be rested to allow the meniscus to heal. Patients take longer to recover from a meniscus suture repair than from a meniscectomy. During the procedure, Dr Lévy will assess the entire joint, looking at the condition of the cartilage in every compartment of the knee, the condition of the cruciate ligaments and the other meniscus.
You will usually be able to go home the same day, with either a cold compression brace (cryo-cuff) for a meniscectomy or a hinged brace for a suture repair. The surgeon will give you an appointment for a check-up in 30 days. You will be able to bear weight on the leg immediately. You should also wear a compression stocking for 30 days. To avoid any clots, a nurse will give you injections of an anticoagulant every day for 10 days.
POSTOPERATIVE CHECK-UPS :
30-DAY CHECK-UP :
Until this appointment you will have to wear a compression stocking (which will have been prescribed in advance) and you should have already begun physiotherapy to restore joint range. The swelling in the knee will have begun to go down and it will be less painful. Dr Lévy will examine the scars and mobility and assess whether there is any residual pain. He will look at your new x-rays and make any necessary adjustments to your recovery plan for the next few months.
3-MONTH CHECK-UP :
Your physiotherapy should nearly be over and the knee should be pain-free. Your muscles will not quite have regained full strength, and you can improve it with either exercises at home or physiotherapy. The surgeon will give you advice to avoid damaging the knee.
REHABILITATION :
Physiotherapy is an important factor for ensuring your knee is pain-free, supple and strong. It will be different depending on whether you had a meniscectomy or a suture repair.
After a meniscectomy, you should expect to regain full flexion quite quickly, and this will be the primary focus before trying to restore muscle strength. After a suture repair, you must mobilise the knee whilst protecting the sutures. You should not bend it more than 90° for 45 days. Therefore, as well as the compression stocking you should wear a hinged brace to prevent you bending the knee too far; you will gradually be able to increase the limits, as explained by your surgeon. It can take a long time to recover from a suture repair and may require several months of physiotherapy before you can resume pivoting sports (average 6 months). After a meniscectomy, you can resume sports after 3–4 months.
You will be able to walk again immediately after meniscus surgery. After a suture repair, you will wear a hinged brace for 45 days. The amount of time you need to take off work will depend on your job. For office workers, this may be a matter of days. For physical jobs or jobs where you need to stand all day, the average time off work is one month for a simple meniscectomy. This may be longer for a meniscus suture repair. You will be able to drive again a few days after a meniscectomy, but not for 15 days after a suture repair. You must protect the meniscus as much as possible to allow it to recover.
A wide range of complications can occur with surgery. Fortunately, they are very rare and the various appointments before and after the surgery are designed to avoid them or detect them early if they do appear.
As well as the risks common to all types of surgery and the risks of the anaesthesia, there are some specific risks associated with this procedure.
The following complications may occur with meniscus surgery :
SURGICAL SITE HAEMATOMA :
A haematoma is a rare but serious complication. It is more common with suture repairs than with meniscectomies. Haematoma happens when there is bleeding from a small vessel in the knee, filling the space with blood. The knee swells and becomes painful and taut. If it gets too swollen, the surgeon may have to perform a joint aspiration. If it happens again, it may require further arthroscopy to locate the leaking blood vessel and cauterise it.
SURGICAL WOUND INFECTION :
Despite all the precautions taken by the operating team, bacteria may still enter the wound either during the surgery or afterwards, before it is fully healed. This causes compromised healing (redness around the wound), severe pain, a purulent discharge and a persistent fever.
You must tell the surgeon if you see any of these signs and seek emergency treatment.
Dr Lévy will decide whether to wash out the knee arthroscopically and send any samples for testing, so he can prescribe the correct antibiotic for any infection.
PHLEBITIS/PULMONARY EMBOLISM
Despite the preventive anticoagulant treatment given after the surgery and despite wearing compression stockings, a clot may still form in the leg veins (phlebitis) and require an effective dose of anticoagulant therapy for 3–6 months.
JOINT STIFFNESS:
This can develop due to inflammation (algodystrophy) and requires targeted physiotherapy. If there is still limited motion after three months, it could be caused by fibrosis which requires surgery to restore full movement.
RAPID CHONDROLYSIS :
In some cases, arthroscopic surgery can trigger rapid deterioration of the cartilage even if the surgeon made no technical errors. This is a rare cartilage reaction to the instruments being inserted inside the joint. It causes severe pain and early and rapidly destructive damage of the cartilage that can be diagnosed with a standard x-ray. Rapid chondrolysis may eventually require knee replacement surgery. Fortunately it is a rare complication. It usually affects patients whose MRI already shows signs of oedema of the tibial plateau underlying the meniscus tear.
COMPLEX REGIONAL PAIN SYNDROME :
Complex Regional Pain Syndrome, also called algoneurodystrophy, is a condition involving pain and other unpleasant symptoms in a joint after surgery or a fracture. The syndrome may have a neurological cause such as damage to the peripheral nervous system, affecting either the small fibres which protect from pain or heat stimuli, and/or the large fibres which detect tactile stimuli. It causes pain and severe stiffness that can last for up to 18 months. Patients always recover fully. Dr Lévy will diagnose the condition using scintigraphy (a scan) and will support you throughout, in order to treat the painful and unpleasant symptoms.
FAILED SUTURES :
In very rare cases the tear does not heal and the pain persists. This failure is only a partial failure, because some of the tear will nevertheless have healed. A new operation will be needed to remove the part that has not healed.
This list does not cover all the possible risks.
Ask Dr Lévy if you want more information, especially if you have any questions about your particular situation and the advantages, disadvantages and risk/benefit ratio of each procedure.