Shoulder Surgery
Rotator Cuff Tendinitis
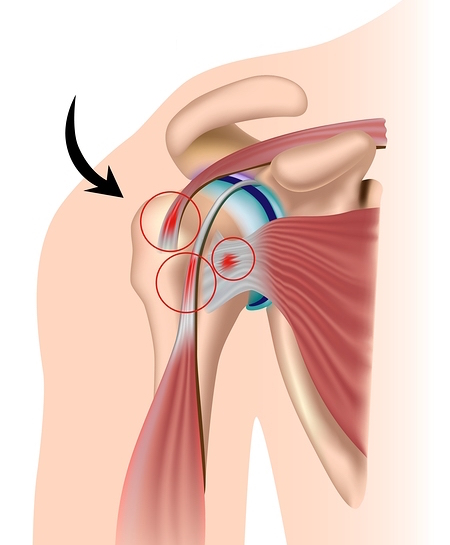
Shoulder tendinitis is inflammation of the rotator cuff tendons, especially the supraspinatus tendon. The pain can be unbearable, and often happens at night. The condition is caused by repetitive movements and could eventually cause the tendons to tear. It happens when the arm is lifted above the shoulder, causing the acromion to rub against the tendon. Treatment may be medical (injections, physical therapy/rehabilitation) or surgical (arthroscopic acromioplasty).
Contents
- Video presentation
- Description & progression
- Surgical indication
- Preparing for surgery
- Hospital stay & procedure
- After the surgery
- Potential complications
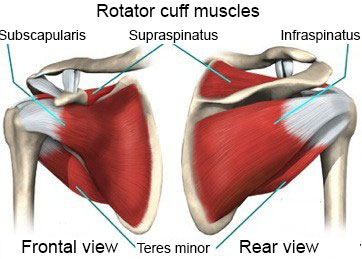
Rotator cuff tendinitis is a very common problem. It happens when one or more of the four shoulder tendons (supraspinatus, infraspinatus, subscapularis or teres minor) gets inflamed.
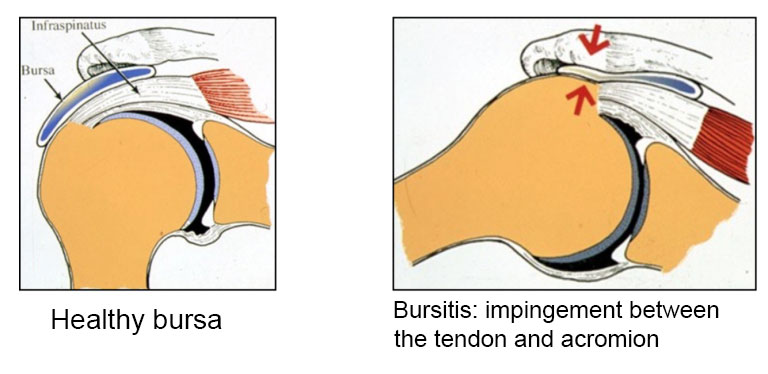
It affects young adults due to the extensive use of these tendons but can also be caused by calcification inside the tendon. The most common cause is excessive friction between the tendons and the acromion (top of the shoulder blade which may rub against the tendons to varying degrees). This rubbing is known as subacromial impingement.
In fact, the acromion may even have a sharp bony spur (hooked acromion) that slices the tendon every time the arm is lifted, causing rotator cuff tendinitis that can even develop into a torn tendon. An early diagnosis is important to avoid residual pain. Treatment involves targeting the inflammation with injections plus physical therapy. If medical treatment fails, the next option is arthroscopic rotator cuff decompression surgery to shave off the sharp spur.
The symptoms of tendinitis in one or more tendons are pain, loss of active movement and loss of strength in the shoulder. It becomes harder to move the arm and daily activities become painful or even impossible to do.
NIGHT PAIN THAT PREVENTS YOU FROM SLEEPING IS A SERIOUS SIGN
If left untreated, the tendons will tear. A torn rotator cuff almost always requires surgery. It causes irreparable atrophy of the muscles, making recovery much harder. A tear can also spread to the other rotator cuff tendons.
Treatment is designed to prevent this tearing and make the shoulder pain-free, not just for sports but for daily life too.
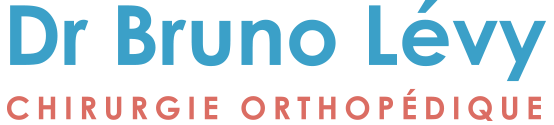
Rotator cuff tendinitis should first be tackled with medical treatment. The surgeon will give you an injection into the shoulder, usually guided by x-ray to get as close to the injury as possible. The injection will reduce the inflammation and therefore stop the tendon rubbing on the acromion. This will be combined with physiotherapy to learn how to lower the shoulder and prevent the impingement between the tendons and the acromion. The exercises will involve subacromial decoaptation (opening the joint space).
If this fails, the next option is surgery. The procedure is known as subacromial decompression or acromioplasty.
Subacromial decompression surgery is essential in the following circumstances:
– Persistent night pain for longer than 6 months, despite having correctly followed the medical treatment (injections and physiotherapy).
– Loss of active movement due to the pain, despite having correctly followed the medical treatment
– Significant loss of strength
SURGICAL CONSULTATION
The aim of the preoperative consultation with the surgeon is to establish a diagnosis. Dr Lévy will examine the shoulder to determine which tendon or tendons are affected. This involves a comprehensive examination to test the tendons one by one and identify which ones are affected by the inflammation.
He will use x-rays and MRIs (or joint scans) to check for any calcification, and especially to make sure there are no torn tendons and quantify the extent of the impingement. This information will be used to plan the surgery. He will explain what will happen during and after the surgery, as well as any potential complications. This will include advice on the length of remission and when you can resume any sports.
If the shoulder is stiff, you may be offered a few sessions of physiotherapy to loosen the joint and prepare the shoulder for the surgery.
ANAESTHETIC CONSULTATION
Once the indications have been confirmed, one of Dr Lévy’s assistants will give you an appointment with the anaesthetist who will look after you during the surgery. The anaesthetist will examine you and prescribe any additional tests that may be needed before the surgery. He or she will also explain how the anaesthesia works. The procedure is always performed under general anaesthesia, together with locoregional anaesthesia to minimise any postoperative pain.
SMOKING
It is essential to stop smoking one month before and after the surgery. This is because a mass influx of nicotine reduces blood flow, slows down the healing process and makes it harder for the tendons to recover. You may use extended-release nicotine patches to help with the withdrawal symptoms.
The surgery will be performed as an outpatient procedure. It usually takes between 30 and 45 minutes.
Subacromial decompression involves shaving off the bony spur on the end of the acromion which is causing the impingement with the tendon. This is done arthroscopically, which means the surgeon does not fully open the joint but instead accesses the space using tiny incisions less than 1cm wide.
Arthroscopy means none of the anatomic structures are affected, and he can access the joint without causing any trauma to the muscles or ligaments. There are many proven benefits of this technique over traditional “open” surgery:
– Little or no visible scarring
– No muscle damage
– Faster functional recovery
– Little or no bleeding
– Less risk of infection.
Two-three tiny incisions will be made around the shoulder, each measuring 5–10mm. An arthroscope (tiny camera) is inserted into one of the incisions so that the surgeon can look at the whole joint, and in particular check there are no torn tendons. Very small instruments are then inserted into the other incisions to perform the surgery. During the procedure, Dr Lévy will check the long head of biceps tendon, the tendon that passes over the shoulder joint. The shoulder does not depend on this tendon for movement, but it can cause severe pain if it is damaged. Dr Lévy then decides whether to perform a tenotomy (careful cutting of the tendon) to alleviate the pain but without affecting the function of the shoulder.
The procedure is demonstrated are shown in the video below. It involves the following successive steps:
– Synovectomy: the shoulder joint is cleaned and the inflamed tissue removed
– Acromioplasty: the acromion is made thinner to stop it impinging on the tendons
– Tenotomy of the long head of biceps tendon: this tendon is very often involved in subacromial impingement, a cause of acute pain
You should keep your arm in a sling night and day for 2–3 weeks after the surgery. If you are very careful or when taking a shower, you can remove your arm from the sling and hold it against your body. You should not raise the arm or actively move it away from the body. Within a few days you can begin a few exercises that involve gently swinging the arm in a pendulum movement. Dr Lévy will explain how to do these exercises properly. He will also prescribe you some sessions of strictly passive physiotherapy, from day 10 after the surgery. The sutures are resorbable and should fall out within 15–20 days. You should then massage the scars to prevent any subcutaneous adhesions from forming.
POSTOPERATIVE CHECK-UPS
30-DAY CHECK-UP
By the time you attend this first check-up, the majority of patients say that the spontaneous night-time pain has disappeared. You should still avoid sleeping on the shoulder but sleep on your back or on your other side. This appointment is the last time you will need to wear the sling. Dr Lévy will make sure the wounds are healing well and check your passive movement. You will have an x-ray to check the acromial hook was cleanly removed. At this point the surgeon will decide whether you can begin active assisted physiotherapy, and increase your passive then active range of motion, depending on the pain. You must continue to massage the scars to prevent any subcutaneous adhesions from forming.
4-MONTH CHECK-UP
At this appointment, Dr Lévy will check the range of motion in all sectors of mobility. It should have increased since the last appointment. By this point, you will usually be able to raise your shoulder between 90–120°. The scars should be soft and you can finally sleep on this side. He will prescribe you further physiotherapy to strengthen the muscles and continue improving your passive range of motion. You will also be shown some exercises that you can do at home every day to stretch the joint.
6-MONTH CHECK-UP
By now the shoulder should be supple and pain-free. The shoulder will not yet have regained full strength, which will gradually return over time. You can resume any sports but should not force the shoulder in case of any residual pain.
A wide range of complications can occur with surgery. Fortunately, they are very rare and the various appointments before and after the surgery are designed to avoid them or detect them early if they do appear.
As well as the risks common to all types of surgery and the risks of the anaesthesia, there are some specific risks associated with this procedure.
The following complications may occur with shoulder decompression surgery:
SURGICAL WOUND INFECTION
Despite all the precautions taken by the operating team, bacteria may still enter the wound either during the surgery or afterwards, before it is fully healed. Signs and symptoms of an infection are compromised healing with severe pain, more redness around the wound than normal, a purulent discharge and a persistent fever.
You must tell the surgeon if you see any of these signs and seek emergency treatment.
COMPLEX REGIONAL PAIN SYNDROME
Complex Regional Pain Syndrome, also known as algodystrophy, is a condition involving pain and other symptoms usually in a limb following trauma or surgery, even if only minor. The syndrome may have a neurological cause such as damage to the peripheral nervous system, affecting either the small fibres which protect from pain or heat stimuli, and/or the large fibres which detect tactile stimuli. It causes pain and severe stiffness that can last for up to 18 months. Patients always recover fully. Dr Lévy will diagnose the condition using scintigraphy (a scan) and will support you throughout, in order to treat the painful and unpleasant symptoms.
This list does not cover all the possible risks.
Ask Dr Lévy if you want more information, especially if you have any questions about your particular situation and the advantages, disadvantages and risk/benefit ratio of each procedure.