Forefoot surgery
Minimally invasive bunion surgery Halluxoplastie®
Dr Lévy performs the halluxoplastie® procedure. He corrects hallux valgus, also known as bunions, using a percutaneous minimally-invasive technique. The halluxoplastie® procedure means less pain after the surgery and a faster recovery than with the standard technique. The scars are practically invisible. It does not involve screws, pins or staples.
Contents
- Video presentation
- Description & progression
- Surgical indication
- Preparing for surgery
- Hospital stay & procedure
- After the surgery
- Recovery period & Return to work
- Potential complications
Hallux valgus (from the Latin hallus = “big toe” and valgus = “turned outwards”) is a deformity of the foot where the first metatarsal deviates inwards (metatarsus varus) and the big toe turns outwards (hallux valgus); it is often accompanied by a bunion (bony bump over the deformity).
Hallux valgus is usually very painful but there is no link between the extent of the deformity and the pain. The pain in the big toe is caused by rubbing against shoes and inflammation of the protruding bony bump (bursitis). It mainly affects women.
There are two types of hallux valgus :
Congenital hallux valgus (30% of cases) :
A hereditary condition transmitted by the father or mother. The deformity appears during childhood and adolescence. It is important to wait until the patient has stopped growing before considering surgery.
Acquired hallux valgus (70% of cases) :
The deformity begins in adulthood. It is caused by failure of the ligaments that stabilise the first metatarsal of the foot. There is probably a hormone element that contributes to the stretching of the ligaments. This is why the condition usually affects women. Footwear probably plays a part in the development of the deformity but is very hard to evaluate to what extent.
Men can also get hallux valgus. It is often linked to being overweight and flat footedness.
Hallux valgus can progress in various ways. The deformity usually gets worse over time and usually starts with very painful inflammatory flare-ups before deteriorating into constant pain.
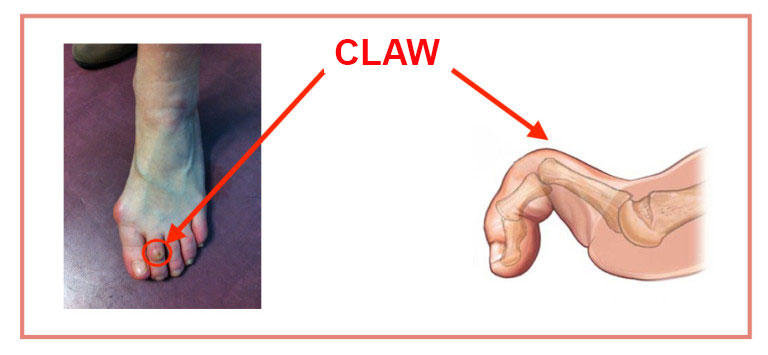
If left untreated, the deformity can in some cases affect the other toes. As it turns outwards, the large toe can push on the second toe, which can develop into a hammer toe or mallet toe. If the deformity persists, the toes may start to overlap, with the second toe lying over or under the big toe.
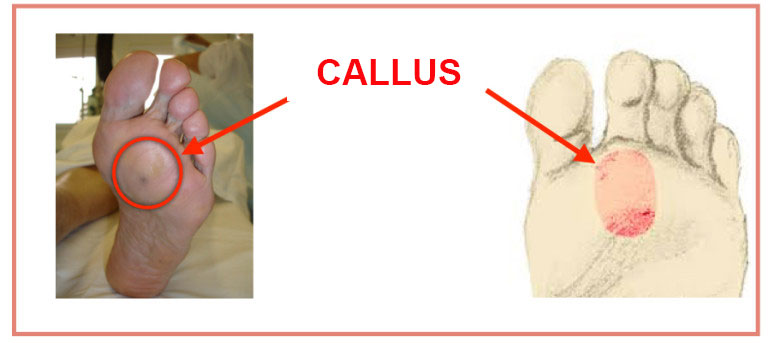
Very often patients complain of pain on the sole of the foot due to excessive pressure on the metatarsals, leading to painful corns on the ball of the foot.
Halluxoplastie® procedure is indicated when there is pain and difficulty wearing shoes..
SPONTANEOUS PAIN :
Felt on the inside edge of the foot over the head of the first metatarsal and the bony bump. It is caused by distension of the medial collateral ligament. The pain is particularly bad at night after a busy day. It can be so bad that even the weight of the sheets on the foot is unbearable.
BURSITIS :
This is caused by the bony bump rubbing against the shoe. The skin turns red and painful. It develops hyperkeratosis (corns), possibly even ulcers and abscesses. They can become infected and lead to arthritis.
DIFFICULTIES WEARING SHOES :
The bump can be painful when wearing tight or high-heeled shoes. Patients may even find it impossible to wear loose-fitting shoes and be forced to wear only sandals or flip-flops.
It is very important to understand that although the deformity may be cosmetically unattractive, this is not a good enough reason for surgery. The surgery is a functional procedure designed to restore normal and pain-free function to the foot. It involves an osteotomy (fracture) of one or more bones to alter the load pattern on the ground. If the surgery is motivated by solely cosmetic reasons, there is a risk of altering the load patterns on the foot resulting in a painful loss of function.
SURGICAL CONSULTATION:
The aim of the preoperative consultation with the surgeon is to establish a diagnosis and analyse the deformity, the loss of function and check for any other pain that the patient may not have mentioned (e.g. plantar pain beneath the second toe). Dr Lévy will examine the structure of your foot to see whether it is flat or hollow. Any deformity will have to be addressed after the surgery using orthopaedic insoles. He will also check for hammer toe or mallet toe, which can be treated at the same time.
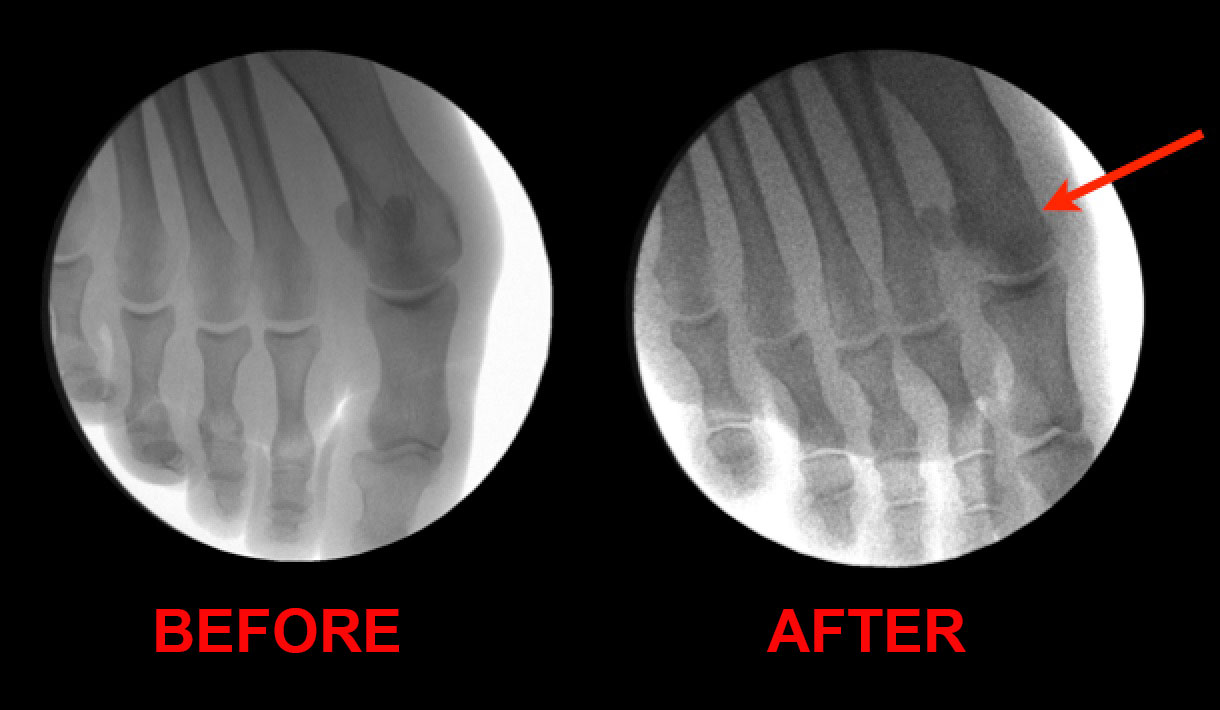
X-rays will be used to help plan the surgery. Dr Lévy will decide what is required based on the deformity and the x-rays. He will explain what will happen during and after the surgery, as well as any potential complications.
ANAESTHETIC CONSULTATION:
Once the indications have been confirmed, one of Dr Lévy’s assistants will give you an appointment with the anaesthetist who will look after you during the surgery. The anaesthetist will examine you and prescribe any additional tests that may be needed before the surgery. He or she will also explain how the anaesthesia works and the best method for you.
SMOKING :
It is essential to stop smoking one month before and after the surgery. This is because a mass influx of nicotine reduces blood flow to the foot and makes it harder for the bone to heal, causing prolonged pain. You may use extended-release nicotine patches to help with the withdrawal symptoms.
Halluxoplastie® procedure is usually carried out as an outpatient procedure (day hospital).
ANAESTHESIA :
The procedure will be performed under local anaesthesia. The anaesthetist will first give you a local anaesthetic into the ankle and top of the foot so you won’t feel any pain or discomfort during the surgery. Further anaesthesia will be given directly into the toes being operated. This top-up is used to prolong the effects of the anaesthesia for 10–12 hours. You will therefore not be in any pain when you return home. When you are discharged from the clinic, you will be given a prescription for pain relief.
PERCUTANEOUS SURGERY :
Dr Lévy will perform the particular procedures needed by each patient (osteotomy, ligament release, cyst removal, treatment for hammer toe or metatarsalgia etc.) using micro-incisions for inserting instruments just 2mm in diameter. He uses a micro-reamer mounted on a motor that spins at 5000 rpm. There are several types of reamer – conical reamers for trimming the protruding bone, and straight reamers to cut the bone like a saw. The procedure does not touch the muscles, tendons or joint capsule. This means there is virtually no pain after the operation and patients can walk again immediately.
Throughout the operation, Dr Lévy will take x-rays to check what is happening and make sure the osteotomy is as accurate as possible.
The scars will be barely visible to the naked eye. With a percutaneous technique, there is no need to detach the muscles, tendons or other structures in contact with the bone in order to perform the osteotomy. There is much less pain after the operation than with traditional surgery, and recovery is much faster.
Once finished, he will apply a compression dressing that will act as a splint for 8–10 days, during which you should not remove or loosen the bandage or get it wet.
You will then spend a few minutes in the recovery room so your vital signs can be monitored, then you can return to your room and wait to be discharged.
Dr Lévy will prescribe any medication needed to alleviate any pain after the surgery. When you are discharged, you will be given a copy of your medical file explaining that you must bring back the dressings to your next check-up, along with any other instructions and the date and time of your next appointment when you will have another x-ray.
After being discharged, you will be able to walk with orthopaedic shoes that Dr Lévy will have prescribed for you during the preoperative consultation.
3D DEMONSTRATION OF THE PROCEDURE :
Dr Lévy will give you an appointment for a check-up in 8–10 days’ time. During this time, you must wear the orthopaedic shoes which are designed to relieve pressure on the forefoot.
POSTOPERATIVE CHECK-UPS :
8–10 DAY CHECK-UP :
Dr Lévy will remove the dressing, check the realignment, examine your x-rays and make sure the wound is healing. He will give you a splint to keep the bones in place and make sure the deformity does not return. This splint will make sure the bone heals in the correct position. You must wear it for 3 weeks. The dressings will be changed every three days until your next appointment. You must wear orthopaedic shoes for one month.
1-MONTH CHECK-UP :
The dressing and splint will be removed. You will return the orthopaedic shoes and can start wearing loose-fitting footwear (e.g. trainers, plimsolls). The swelling usually takes about 3 months to go down. Dr Lévy will give you compression bands which you must wear every day for three months after the operation. He will also give you some exercises to do at home to help recover the full range of motion in your toes.
3-MONTH CHECK-UP :
This is a simple check-up to see how you are doing. However, each case is different and you may be given advice on how to improve your condition and speed up your recovery.
You may also be given further appointments, if the surgeon thinks it is necessary.
REHABILITATION :
The benefit of percutaneous surgery is less stiffness after the procedure. In most cases there is no need for physical therapy/rehabilitation. At your first check-up appointment, Dr Lévy will give you some exercises to do at home. These exercises are designed to restore the range of motion in the joints, massage the scars to prevent any deep-seated adhesions, and get you walking again normally.
In some cases, he may want to prescribe you some sessions with a physiotherapist.
The length of time you need to take off work will depend on your job and how you travel to get there. Due to the osteotomy, there will be swelling for about three months after the surgery.
You should not drive for six weeks (unless you have an automatic car and operate the pedals using the other foot). Likewise, you should not expect to be able to walk for long distances for at least six weeks.
For example, if you work in an office located 5 minutes from your house, you can expect to return to work within a month, or possibly even one week after the surgery. On the other hand, if you have a physically active job with a 2-hour daily commute, you may need to take up to three months off. These are just two examples, and your situation may lie anywhere in between.
A wide range of complications can occur with surgery. Fortunately, they are very rare and the various appointments before and after the surgery are designed to avoid them or detect them early if they do appear.
As well as the risks common to all types of surgery and the risks of the anaesthesia, there are some specific risks associated with this procedure.
The following complications may occur with percutaneous surgery of the foot:
SURGICAL WOUND INFECTION :
Despite all the precautions taken by the operating team, bacteria may still enter the wound either during the surgery or afterwards, before it is fully healed. Signs and symptoms of an infection are compromised healing with severe pain, more redness around the wound than normal, a purulent discharge and a persistent fever.
You must tell the surgeon if you see any of these signs and seek emergency treatment.
NEURAPRAXIA :
During the operation, the surgeon will be working closely to the sensory nerves in the toes. If the instruments get too hot when close to these nerves, they may suffer a refractory period when feeling in one or more toes may lessen or disappear. This loss of feeling does not cause any problems when wearing shoes, and usually recovers within a year after the surgery.
DELAYED HEALING:
Sometimes, the bones take longer than three months to heal. This is often the case with smokers who were unable to quit before, during and/or after the surgery due to the decreased blood flow to the toes. In these cases, Dr Lévy will give you advice on how to reduce pressure on the bones and help them heal faster.
PHLEBITIS/PULMONARY EMBOLISM :
Despite being able to walk again immediately, a clot may form in one of the veins of your leg (phlebitis) and require an effective dose of anticoagulant treatment for 3–6 months. This complication is rare with percutaneous surgery because the patient can walk again the same day.
COMPLEX REGIONAL PAIN SYNDROME :
Complex Regional Pain Syndrome, also known as algodystrophy, is a condition involving pain and other symptoms usually in a limb following trauma or surgery, even if only minor. The syndrome may have a neurological cause such as damage to the peripheral nervous system, affecting either the small fibres which protect from pain or heat stimuli, and/or the large fibres which detect tactile stimuli. It causes pain and severe stiffness that can last for up to 18 months. Patients always recover fully. Dr Lévy will diagnose the condition using scintigraphy (a scan) and will support you throughout, in order to treat the painful and unpleasant symptoms.
LOAD TRANSFER AND METATARSALGIA:
With some foot shapes (Greek foot, where the second toe is longer than the big toe), the change in loading pattern resulting from the surgery places excessive load on the second toe, causing plantar pain under the second metatarsal (metatarsalgia). This can be treated with orthopaedic insoles and further surgery to correct the excessive load. Dr Lévy should usually be able to detect this foot shape before the surgery and anticipate the load transfer to the second toe. However, this is sometimes not enough and the metatarsalgia can still occur.
RELAPSE :
In rare cases, the deformity can return, especially if the patient has flat feet or wears very tight shoes. The surgeon will give you advice on how to prevent this happening. If necessary, you will be prescribed orthopaedic insoles.
This list does not cover all the possible risks.
Ask Dr Lévy if you want more information, especially if you have any questions about your particular situation and the advantages, disadvantages and risk/benefit ratio of each procedure.