Knee surgery
Total Knee Replacement
Osteoarthritis of the knee is a degenerative condition that affects the knee joint. It causes increasing degrees of knee pain, which gradually reduces the distance a person can walk. It becomes harder to bend the knee, leading to a loss of independence. There are many treatments to slow down this condition (e.g. injections, viscosupplementation). A knee replacement is the last resort and involves surgery to replace the knee with a prosthetic joint.
Contents
- Page information
- Description & progression
- Diagnosis & Surgical indication
- Preparing for surgery
- Hospital stay & procedure
- After the surgery & Results
- Potential complications
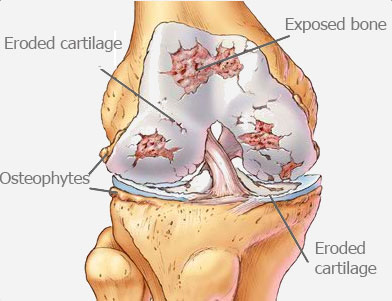
Osteoarthritis of the knee happens when the surfaces inside the knee joint become worn down and the cartilage gradually disappears. This wearing away gets worse over time, causing abnormal friction, pain, swelling (fluid accumulation) and stiffness in the joint (limited flexion and extension). The wearing away of the cartilage is irreversible and there is no cure for osteoarthritis. The only thing you can do is slow it down.
Some of the clinical signs can be very disabling for day-to-day life:
- Reduced walking distance
- Difficulties with stairs, especially when coming down
- Difficulties getting up from an armchair or low seat
- Pain at night
- Episodes of “locked knee”
Osteoarthritis is a degenerative condition which means it is linked to wear and tear, but there are also extrinsic factors that can accelerate the progression of the disease. The main causes are:
- An anterior cruciate ligament tear (which can cause meniscus tears and cartilage damage)
- Knee surgery (especially a meniscectomy)
- Fractures (tibia, femur or patella) or patellar dislocation
- A rheumatic disorder (e.g. chondrocalcinosis, rheumatoid arthritis)
- Joint malalignment (genu varum or genu valgum)
The first step in treating osteoarthritis is to give medical treatment i.e. pain relief. This is often combined with hygiene and dietary measure to alleviate the pain. Patients are often advised to lose weight and do regular exercise (such as swimming, cycling or general physical therapy to increase muscle strength). Orthopaedic insoles may also help to realign the knee. Injections of hyaluronic acid will also be required to lubricate the joint and protect the damaged cartilage.
If medical treatment is no longer having the desired effect, the only way to relieve the pain is with surgery. There are various procedures available:
- Realignment osteotomy (usually a valgus-producing osteotomy)
- Unicompartmental knee replacement (UKR)
- Total Knee Replacement (TKR)
The condition is diagnosed based on the clinical history, with patients often clearly describing pain for many years, swelling, a gradual reduction in the distance they are able to walk, initially when going up or down stairs and when walking on uneven ground, and eventually when walking on flat ground.
An x-ray is essential for confirming the diagnosis. The images are taken with the patient standing upright on both legs, which gives a good indication of what happens when they walk. The images will reveal joint impingement (a narrowing of the distance between the joint surfaces) indicating loss of the cartilage. X-rays will also be taken of the whole leg and with the patient in the Schuss position to measure the damage to the cartilage.
An MRI or joint scan may also be requested for certain cases but will never replace the x-rays.
Osteoarthritis may affect one of three joint spaces inside the knee: the medial compartment, the lateral compartment (both located between the femur and the tibia), or the patellofemoral compartment (located between the femur and the patella). Severe cases may affect two or even all three spaces.
A Total Knee Replacement is indicated when two or three compartments are affected and medical treatment no longer has any effect. The procedure offers functional treatment with the sole aim of improving the patient’s quality of life. It is therefore ultimately up to the patient to decide whether to go ahead with the operation. Dr Lévy will try to explain what will happen in either scenario, with and without the surgery. The operation is recommended for patients whose daily lives are being affected by disabling pain in the knee. This disability should be significant, and not just occasional. There is no hard and fast rule, because every patient is different. There is no age limit for a total knee replacement, but it should be avoided in young patients because the only limitation of the procedure is the life span of the implants, which will eventually have to be replaced if the patient is too young; although sometimes, there is obviously no other option. Fortunately, there have been great improvements in implant quality and they now have a much longer life span.
Ultimately, the need for surgery will be decided after a long discussion between the patient and surgeon.
SURGICAL CONSULTATION:
The aim of the preoperative consultation with the surgeon is to establish a diagnosis. Dr Lévy will examine the knee to assess the damage to the different compartments. He will analyse the patient’s gait (to check for any limp), joint flexion, and whether there is a lack of full extension (a flexion contracture); the examination will also look for any ligament laxity. The surgeon will check for any vascular problems in the legs by feeling for the pulses.
X-rays and other test results will be used to help plan the surgery. Depending on the damage and its cause, Dr Lévy will decide what is required. He will explain what will happen during and after the surgery, as well as any potential complications. This will include a discussion of how long the treatment will last, the recovery time and any rehabilitation required after the operation.
You will be given time to discuss your options, and you will receive advice on the pros and cons of the surgery.
Once a decision has been made, Dr Lévy will take some blood and urine samples in order to make sure you have no infections. He will also ask for an x-ray of your teeth to rule out a dental infection. You will have to see a cardiologist and get their go-ahead for the surgery. Finally, you will have an appointment with the anaesthetist.
ANAESTHETIC CONSULTATION:
Once the indications have been confirmed, one of Dr Lévy’s assistants will give you an appointment with the anaesthetist who will look after you during the operation. The anaesthetist will examine you and prescribe any additional tests that may be needed before the surgery. He or she will also explain how the anaesthesia works and the best method for you. The procedure is usually carried out under general anaesthesia.
SMOKING :
Once the indications have been confirmed, one of Dr Lévy’s assistants will give you an appointment with the anaesthetist who will look after you during the operation. The anaesthetist will examine you and prescribe any additional tests that may be needed before the surgery. He or she will also explain how the anaesthesia works and the best method for you. The procedure is usually carried out under general anaesthesia.
You will stay in hospital for about a week. This time will be used to treat the initial pain, monitor the wound and start your rehabilitation.
The procedure is usually performed under general anaesthesia. It takes about 90 minutes. The surgeon will make an incision in the knee in front of the joint, starting at the base of the thigh, crossing over the kneecap and ending at the top of the shin. Next, any remaining cartilage will be removed in order to create space for the prosthetic joint. The height of the removed cartilage is measured to ensure the implant is as accurate as possible. He can then select the perfect size implant for each patient. He uses cutting guides and ultra-precision instruments to place the implant in exactly the right position, based on the plans made in advance.
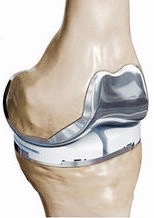
There are four parts to the implant:
- A femoral component made from chrome/cobalt, which gets fixed to the femur
- A tibial component made from chrome/cobalt, which gets fixed to the tibia
- A patellar component made from polyethylene, which gets fixed to the kneecap and slides against the femoral component
- A polyethylene insert that sits between the femoral component and the tibial component
The surgeon will also carefully correct any malalignment in the joint, if necessary. He will carefully secure haemostasis (cauterise the blood vessels) to keep the blood loss to a minimum. A process called autologous blood transfusion is often used – the blood shed during the surgery is centrifuged, concentrated, then reinfused back into the patient to avoid the need for a subsequent blood transfusion. Autologous transfusions are safe because they use the patient’s own blood. There is therefore no risk of contamination or rejection.
Once the operation is finished, you will be transferred to the recovery room where your vital signs and pain levels will be monitored. Any autologous transfusion will take place in the recovery room. You will spend about two hours there.
Then you will return to your room to rest. The next day, the nurses will administer any painkillers prescribed by the anaesthetist, and you will receive a visit from the physiotherapist to start your rehabilitation. The exercises will initially focus on contracting the quadriceps muscles. This will be followed by flexion exercises. You will receive a private physiotherapy session every day. For some of the first day, you will be allowed to sit up in a chair.
You will usually be able to try standing on the second day; after that you can take a few steps, first with a walker then with two crutches.
As you improve, you will attempt walking up and down stairs.
You will usually be discharged to a rehabilitation centre for several weeks, but you may also be allowed to return home and receive daily visits by nurses, support workers and physiotherapists under the PRADO protocol, a scheme introduced by the Department of Social Security to help patients return home after an operation.
During the first month you will be allowed to walk as much as you like without limits. Rehabilitation will start as soon as possible, with the aim of restoring full extension in the joint. It will take longer to restore full flexion. The nursing team will also give you injections of anticoagulants (for 30 days) and change your dressings. You should do your exercises every day to help your knee recover as much flexion as possible. The skin staples will be removed on day 21.
POSTOPERATIVE CHECK-UPS :
30-DAY CHECK-UP :
Until this appointment you will have to wear compression stockings (which will have been prescribed in advance) and you should have already begun physiotherapy to restore joint range. The swelling in the knee will have begun to go down a little bit, and it will be less painful. Dr Lévy will examine the scar, your mobility, and determine whether there is any residual pain. He will look at your new x-rays and make any necessary adjustments to your recovery plan for the next few months. You should be able to start driving again after 30–45 days.
4-MONTH CHECK-UP :
Physiotherapy will now focus on strengthening the quadriceps muscles to stabilise the knee. You should be getting used to your implant but will still be aware it is there. Your muscles may not quite have regained full strength, which can be improved with either exercises at home or physiotherapy. The surgeon will give you advice to avoid damaging the knee.
If your knee is stable and the quadriceps nicely toned, Dr Lévy will allow you to resume cycling and swimming.
12-MONTH CHECK-UP :
In principle, you should no longer be in any pain and be able to walk as much as you want. However, each knee is different and Dr Lévy will give you specific advice on whether you can resume your particular sport. It is possible to play many sports after a total knee replacement (e.g. tennis, golf, skiing, running). Contact sports (e.g. football, rugby, judo) should be avoided.
RESULTS :
The results of knee replacement surgery are excellent in over 90% of cases, with patients experiencing no or very mild pain. However, a total knee replacement does not give you back your original knee, and you will always be aware that you have a prosthetic joint. Nevertheless, it should not cause you any discomfort. You will simply be aware it is there from time to time.
The average life span of a total knee replacement is 15 years. After this time it will need to be replaced. The operation is often more complicated than the first time, and the results not quite as good.
You should see your surgeon for a check-up every year, with x-rays to check for any complications. This will just be a short appointment so the surgeon can check the scar, your movement, any pain and the x-rays.
You must take every precaution against infections and treat any infection as quickly as possible (dental, sinus, urinary infections etc.). This is because the bacteria could migrate to the shoulder at any time and infect the implant, in which case the only option will be to have it replaced.
A wide range of complications can occur with surgery. Fortunately, they are very rare and the various appointments before and after the surgery are designed to avoid them or detect them early if they do appear.
As well as the risks common to all types of surgery and the risks of the anaesthesia, there are some specific risks associated with this procedure.
The following complications may occur with knee replacement surgery:
SURGICAL SITE HAEMATOMA :
A haematoma is a rare but serious complication. It happens when there is bleeding from a small vessel in the knee, filling the space with blood. The knee swells and becomes painful and taut. If it gets too swollen, the surgeon may have to perform a joint aspiration. If it happens again, it may require further surgery to locate the leaking blood vessel and cauterise it.
SURGICAL WOUND INFECTION :
Despite all the precautions taken by the operating team, bacteria may still enter the wound either during the surgery or afterwards, before it is fully healed. This compromises the healing (more redness around the wound than normal), causing severe pain, a purulent discharge and a persistent fever.
You must tell the surgeon if you see any of these signs and seek EMERGENCY treatment.
DO NOT TAKE ANY ANTIBIOTICS BEFORE SEEING THE SURGEON.
Dr Lévy will decide whether to wash out the knee and take samples for testing so that he can prescribe the correct antibiotic, assuming the infection has been caught in time. Otherwise, the implant will have to be replaced. This is a major operation to treat the infection and can mean the functional results are not as good as was originally expected. You will also have to take antibiotics for at least 45 days and have regular check-ups with the surgeon. It is a serious complication.
PHLEBITIS/PULMONARY EMBOLISM :
Despite the preventive anticoagulant treatment given after the surgery and despite wearing compression stockings, a clot may still form in the leg veins (phlebitis) and require long-term curative anticoagulant therapy.
JOINT STIFFNESS :
This can be a knock-on effect of inflammation (algodystrophy) and requires targeted physiotherapy. If you have not regained your full range of motion after three months, it could be caused by fibrosis which requires surgery.
COMPLEX REGIONAL PAIN SYNDROME :
Complex Regional Pain Syndrome, also called algoneurodystrophy, is a condition involving pain and other unpleasant symptoms in a joint after surgery or a fracture. The syndrome may have a neurological cause such as damage to the peripheral nervous system, affecting either the small fibres which protect from pain or heat stimuli, and/or the large fibres which detect tactile stimuli. It causes pain and severe stiffness that can last for up to 18 months. Patients always recover fully. Dr Lévy will diagnose the condition using scintigraphy (a scan) and will support you throughout, in order to treat the painful and unpleasant symptoms.
IMPLANT LOOSENING :
This is not a complication but a natural problem as the implant gets older. After several years, the implant can become loose and cause pain. It will need to be replaced. An undetected infection could cause an implant to loosen sooner than expected. This is known as septic loosening. The surgeon will always check for an infection in case of early loosening.
This list does not cover all the possible risks.
Ask Dr Lévy if you want more information, especially if you have any questions about your particular situation and the advantages, disadvantages and risk/benefit ratio of each procedure.