Home » Pathologies » Knee Surgery » Anterior Cruciate Ligament Tear
Anterior Cruciate Ligament Tear
A torn anterior cruciate ligament is a very common injury following trauma to the knee. It usually happens in sporting accidents (e.g. skiing, football). It causes very sharp pain, bleeding in the joint (haemarthrosis) and instability (feeling of the knee being loose).
Treatment is usually arthroscopic surgery involving a tendon graft to reconstruct the anterior cruciate ligament.
Video of the procedure
Description & progression
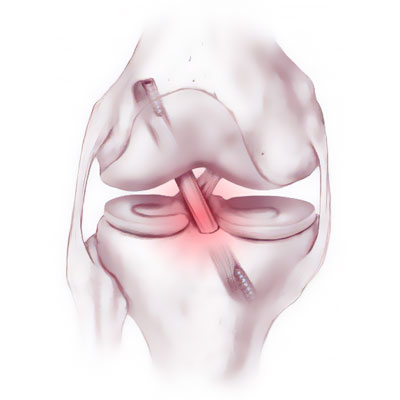
There are four main ligaments that give stability to the knee.
The collateral ligaments, which sit just beneath the skin on either side of the knee (medial and lateral collateral ligaments) and provide frontal plane stability.
The cruciate ligaments which are inside the joint (anterior and posterior cruciate ligaments) and provide stability in the sagittal plane.
The anterior cruciate ligament links the anterior part of the tibia to the posterior part of the femur. It stops the tibia from sliding out in front of the femur and stabilises the knee during rotation.
The anterior cruciate ligament can tear during an accident (playing sport, at work or at home) and lead to a knee sprain. It often involves a high degree of trauma. The most common causes are skiing and football accidents. There are around 20,000 cases each year in France. The knee twists and the patient often both feels and hears a short but sharp snap.
At first the pain is very bad and the patient feels the knee give out. After a few seconds, the patient can stand but is unable to place any weight on the leg, which is too unstable.
In the minutes or hours after the trauma, the knee begins to swell badly due to bleeding inside the joint caused when the blood vessels ripped. This bleeding inside the joint is called haemarthrosis.
The injury may be accompanied by a meniscus tear or damage to one or both of the collateral ligaments.
PROGRESSION :
The ligament is unable to heal itself and restore the anatomy to normal. If left untreated, the knee will usually remain loose and continue to give way, which may get worse over time. With a loose knee, any pivoting movements during sport risk causing further episodes of instability, which feel like a new sprain, and the looseness may lead to progressive meniscus tear or damage to the cartilage (osteoarthritis).
Surgical indication
The decision to offer surgery (ligamentoplasty) depends on the patient’s age, participation in sports and whether there is any instability.
A desire to continue participating in pivoting sports is justification for surgery to reconstruct the anterior cruciate ligament (ligamentoplasty) and thus to stabilise the knee, avoiding any secondary damage and deterioration in the joint.
Young patients (although there is no clear cut-off age) may have a ligamentoplasty to avoid any meniscus tear or cartilage damage. In fact, the age at which the injury was sustained will determine the number of years during which the knee will continue to be subjected to sporting stresses.
Not every torn anterior cruciate ligament will necessarily need surgery.
The surgeon will advise the best approach for your particular anterior cruciate ligament injury. Some athletes are in fact able to resume full sports after a ligament tear thanks to extensive physiotherapy or remarkable adaptability.
Even if the joint is lax, some non-pivoting sports (cycling, jogging) may still be possible.
Preparing for surgery
SURGICAL CONSULTATION:
The aim of the preoperative consultation with the surgeon is to establish a diagnosis. Dr Lévy will examine the knee to determine how much the cruciate ligament is damaged. This will involve a full examination of the knee to check for any meniscus tear or other ligament laxity.
X-rays and an MRI will be used to help plan the surgery.
Depending on the damage and its cause, Dr Lévy will decide what is required. He will explain what will happen during and after the surgery, as well as any potential complications. This will include advice on the length of remission and when you can resume any sports.
ANAESTHETIC CONSULTATION:
Once the indications have been confirmed, one of Dr Lévy’s assistants will give you an appointment with the anaesthetist who will look after you during the surgery. The anaesthetist will examine you and prescribe any additional tests that may be needed before the surgery. He or she will also explain how the anaesthesia works and the best method for you. The procedure is usually performed under general anaesthesia, with a regional catheter in the thigh for reducing the pain immediately after the procedure.
SMOKING :
It is essential to stop smoking one month before and after the surgery. This is because a mass influx of nicotine reduces blood flow, slows down the healing process and makes it harder for the new cruciate ligament to fuse with the bone. You may use extended-release nicotine patches to help with the withdrawal symptoms.
Hospital stay & procedure
The surgery will be performed as an outpatient procedure. Dr Lévy preforms most ligamentoplasties using the 4-strand semitendinosus technique (ST4) and a short graft. The graft is harvested using a short 2cm incision over the inside edge of the tibia.
The rest of the procedure is performed arthroscopically (guided using a camera). The surgeon makes tunnels in the tibia and femur using special instruments. These tunnels are positioned exactly at the insertion points of the torn cruciate ligament. The graft is carefully measured then the tunnels made exactly the same size. The graft is secured using two anchors fixed to the femur and tibia. These anchors support the graft until it has fused with the bone.
You will be able to get out of bed either the same evening or the next morning, depending on the time of your surgery. You will wear a soft knee brace for 15 days to provide initial support and assistance for your knee.
This video demonstrates the procedure:
After the surgery
During the first month you will be allowed to walk as much as you like without limits. Rehabilitation will start as soon as possible, with the aim of restoring full extension in the joint. It takes longer to restore full flexion. The nursing team will also give you injections of anticoagulants (for 15 days) and change your dressings.
POSTOPERATIVE CHECK-UPS AND REHABILITATION :
30-DAY CHECK-UP :
Until this appointment you will have to wear a compression stocking (which will have been prescribed in advance) and you should have already begun physiotherapy to restore joint range. The swelling in the knee will have begun to go down, and it will be less painful. Dr Lévy will examine the scar and your mobility and assess whether there is any residual pain. He will look at your new x-rays and make any necessary adjustments to your recovery plan for the next few months.
Depending on your recovery, you may be allowed to resume cycling (on an exercise bike) and swimming (kicking the legs only).
4-MONTH CHECK-UP :
Physiotherapy will now focus on strengthening the quadriceps muscles to stabilise the knee, encouraging integration and synovial coverage of the new ligament. Your knee should feel completely normal during day-to-day activities. Your muscles will not quite have regained full strength, and you can improve it with either exercises at home or physiotherapy. Dr Lévy will give you advice to avoid damaging the knee.
If your knee is stable and the quadriceps nicely toned, he will allow you to resume straight-ahead running on flat ground.
6-MONTH CHECK-UP :
However, each knee is different and Dr Lévy will give you specific advice on whether you can resume your particular sport or whether you need to continue rehabilitation.
Unless you are an elite athlete who receives daily care from sports physiotherapists and their coaches, it is unlikely you will be able to resume pivoting sports by this point. You will usually have to wait 8–10 months.
Recovery period & Return to work
You will be able to walk again immediately after an anterior cruciate ligament repair. You will need to wear a brace for 15 days.
If you also had a suture repair, you will wear a hinged brace for 45 days.
The amount of time you need to take off work will depend on your job.
For office workers, this may be a matter of days.
For physical jobs or jobs where you need to stand all day, the average time off work one month. This may be longer if the surgeon also had to repair a meniscus tear.
You can resume driving after a few days. However, you may need to spend even longer off work if your job is incompatible with your recovery.
Potential complications
A wide range of complications can occur with surgery. Fortunately, they are very rare and the various appointments before and after the surgery are designed to avoid them or detect them early if they do appear.
As well as the risks common to all types of surgery and the risks of the anaesthesia, there are some specific risks associated with this procedure.
The following complications may occur with arthroscopic ligament reconstruction surgery :
SURGICAL SITE HAEMATOMA :
A haematoma is a rare but serious complication. It happens when there is bleeding from a small vessel in the knee, filling the space with blood. The knee swells and becomes painful and taut. If it gets too swollen, the surgeon may have to perform a joint aspiration. If it happens again, it may require further arthroscopy to locate the leaking blood vessel and cauterise it.
SURGICAL WOUND INFECTION :
Despite all the precautions taken by the operating team, bacteria may still enter the wound either during the surgery or afterwards, before it is fully healed. This causes compromised healing (more redness around the wound than normal), severe pain, a purulent discharge and a persistent fever.
You must tell the surgeon if you see any of these signs and seek emergency treatment.
Dr Lévy will decide whether to wash out the knee arthroscopically and send any samples for testing, so that he can prescribe the correct antibiotic for any infection.
PHLEBITIS/PULMONARY EMBOLISM :
Despite the preventive anticoagulant treatment given after the surgery and despite wearing compression stockings, a clot may still form in the leg veins (phlebitis) and require an effective dose of anticoagulant therapy for 3–6 months.
JOINT STIFFNESS :
This can develop due to inflammation (algodystrophy) and requires targeted physiotherapy. If there is still limited motion after three months, it could be caused by fibrosis which requires surgery to restore full movement.
COMPLEX REGIONAL PAIN SYNDROME :
Complex Regional Pain Syndrome, also called algoneurodystrophy, is a condition involving pain and other unpleasant symptoms in a joint after surgery or a fracture. The syndrome may have a neurological cause such as damage to the peripheral nervous system, affecting either the small fibres which protect from pain or heat stimuli, and/or the large fibres which detect tactile stimuli. It causes pain and severe stiffness that can last for up to 18 months. Patients always recover fully. Dr Lévy will diagnose the condition using scintigraphy (a scan) and will support you throughout, in order to treat the painful and unpleasant symptoms.
RE-TEAR :
The new ligament is almost equally at risk of tearing against as the ligament in your other knee, especially if you resume the same sports.
This list does not cover all the possible risks.
Ask Dr Lévy if you want more information, especially if you have any questions about your particular situation and the advantages, disadvantages and risk/benefit ratio of each procedure.