Home » Pathologies » Shoulder Surgery » Rotator Cuff Tear
Rotator Cuff Tear
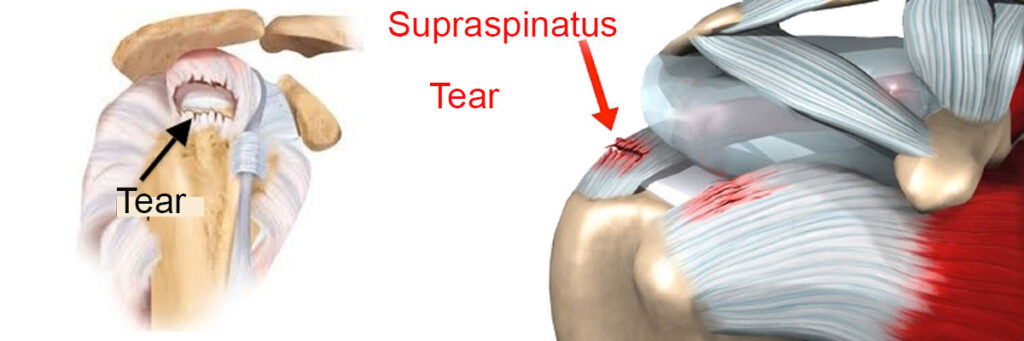
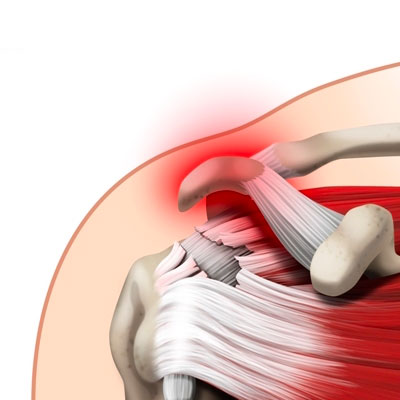
A rotator cuff tear is when the tendons used to move the shoulder joint get torn. The tear may be degenerative (wear and tear caused by repetitive movements; deterioration of rotator cuff tendinitis) or due to trauma (after a fall or inadvertent movement).
It causes pain, weakness and loss of mobility in the shoulder. Treatment may be medical (injections, physical therapy/rehabilitation) or surgical (arthroscopic reconstruction).
Presentation video
Description & progression
A torn rotator cuff is a very common problem. It happens when one or more of the four shoulder tendons (supraspinatus, infraspinatus, subscapularis or teres minor) gets torn.
It affects adults over 40 either as a result of a degenerative tendon condition and/or trauma (direct impact, sprain, dislocation). An early diagnosis is important to avoid residual pain. under general anaesthetic and is performed as an oupatient procedure.
There are two types of rotator cuff tear:
Traumatic (dislocated shoulder, a violent forced movement causing the shoulder to snap)
Degenerative (wear, ageing), although the two types are often interlinked.
The symptoms of a torn tendon are pain, loss of active movement and loss of strength in the shoulder. It becomes harder to move the arm, and daily activities become painful or even impossible to do.
THE MAIN SIGN IS NIGHT PAIN THAT PREVENTS YOU FROM SLEEPING
If you leave it too long without treatment, the tendons shrink (making the surgery more complicated) and the muscles irreversibly waste away, meaning you are less likely to recover fully. A tear can also spread to the other rotator cuff tendons. The aim of repairing the rotator cuff is to alleviate the pain and restore mobility and strength to the shoulder. It will also prevent progressive deterioration of the joint and its function.
Surgical indication
For a traumatic tear (especially if the patient is young), surgery is unavoidable. The sooner it is repaired, the simpler the operation and recovery.
For degenerative tears, treatment is discussed on a case-by-case basis. It depends on the clinical signs (pain, loss of function, loss of strength, age). Small partial or total tears may only need an injection together with physiotherapy. Surgical repair is only offered if this approach fails.
Surgical repair is essential in the following circumstances:
- Persistent night pain despite having correctly followed the medical treatment (injections and physiotherapy)
- Young age (<60 years)
- Loss of active mobility (pseudo-frozen shoulder = shoulder easily mobile in passive motion but has lost active movement)
- Significant loss of strength
- Damage to the subscapularis tendon
Preparing for surgery
SURGICAL CONSULTATION
The aim of the preoperative consultation with the surgeon is to establish a diagnosis. Dr Lévy will examine the shoulder to determine which tendon or tendons are affected. This involves a comprehensive examination to test the tendons one by one and identify which ones are affected by the tear.
He will look at X-rays and an MRI (or joint scan) to quantify the tear, muscle quality and retraction. This information will be used to plan the surgery. Depending on the damage and its cause, Dr Lévy will decide what is required.
He will explain what will happen during and after the surgery, as well as any potential complications. This will include advice on the length of remission and when you can resume any sports.
If the shoulder is stiff, you may be offered a few sessions of physiotherapy to loosen the joint and prepare the shoulder for the surgery.
ANAESTHETIC CONSULTATION:
Once the indications have been confirmed, one of Dr Lévy’s assistants will give you an appointment with the anaesthetist who will look after you during the surgery. The anaesthetist will examine you and prescribe any additional tests that may be needed before the surgery. He or she will also explain how the anaesthesia works. The procedure is always performed under general anaesthesia, together with locoregional anaesthesia to minimise any postoperative pain.
SMOKING :
It is essential to stop smoking one month before and after the surgery. This is because a mass influx of nicotine reduces blood flow, slows down the healing process and makes it harder for the tendons to fuse with the bones. You may use extended-release nicotine patches to help with the withdrawal symptoms.
Hospital stay & procedure
The surgery will be performed as an outpatient procedure. It will take between 45–90 minutes, depending on the complexity of the tear and number of tendons to repair.
A rotator cuff repair involves reattaching the torn tendon to its anatomic site in order to restore function. This is done arthroscopically, which means the surgeon does not open up the entire joint but instead accesses it using tiny incisions less than 1cm wide.
Arthroscopy means none of the anatomic structures are affected, and Dr Lévy can access the joint without causing any trauma to the muscles or ligaments. There are many proven benefits of this technique over traditional “open” surgery:
- Little or no visible scarring
- No muscle damage
- Faster functional recovery
- Little or no bleeding
- Less risk of infection.
Several tiny incisions will be made around the shoulder, each measuring 5–10mm. An arthroscope (tiny camera) is inserted into one of the incisions so that the surgeon can look at the whole joint, and in particular the torn tendons. Very small instruments are then inserted into the other incisions to perform the surgery.
The procedure is demonstrated in the video below. It involves the following successive steps:
- Synovectomy: the shoulder joint is cleaned and the inflamed tissue removed
- Stripping the bone and tendon to prepare for the repair and help them heal faster
- Acromioplasty: removing a small bit of the bone above the tendons (acromion) to avoid any impingement with the newly-sutured tendon.
- Attaching one or more anchors, screwed to the humerus. Threads are attached to the anchors and passed through the tendon. They are then tied to secure the tendon to the bone and create the necessary bone/tendon contact for the structures to heal.
- Double fixation by attaching the threads to a second row of anchors in order to ensure the repair is secure and increase the contact area between the tendon and bone.
There are several ways of repairing the tendons using impacted or screwed anchors, sutures or suture strips. Dr Lévy will decide the best technique based on each particular tear.
After the surgery
 You should keep your arm in a sling day and night for one month after the surgery. If you are very careful or when taking a shower, you can remove your arm from the sling and hold it against your body. You should not raise the arm or actively move it away from the body. Depending on the complexity, Dr Lévy may give you some exercises involving strictly passive movement, starting 10 days after the operation. If the repair was tricky and the tendons particularly retracted, physiotherapy will start after the one-month check-up. In all cases, Dr Lévy will ask you to do some pendulum exercises to prevent the shoulder getting stiff.
You should keep your arm in a sling day and night for one month after the surgery. If you are very careful or when taking a shower, you can remove your arm from the sling and hold it against your body. You should not raise the arm or actively move it away from the body. Depending on the complexity, Dr Lévy may give you some exercises involving strictly passive movement, starting 10 days after the operation. If the repair was tricky and the tendons particularly retracted, physiotherapy will start after the one-month check-up. In all cases, Dr Lévy will ask you to do some pendulum exercises to prevent the shoulder getting stiff.
POSTOPERATIVE CHECK-UPS :
30-DAY CHECK-UP :
By the time you attend this first check-up, the majority of patients say that the spontaneous night-time pain has disappeared. You should still avoid sleeping on the shoulder but sleep on your back or on your other side. This appointment is the last time you will need to wear the sling. Dr Lévy will make sure the wounds are healing well and check your passive movement. An x-ray will be used to check that the implants used to secure your tendons have stayed in place. At this point the surgeon he whether you can begin active assisted physiotherapy, and increase your passive then active range of motion, depending on the pain. You must continue to massage the scars to prevent any subcutaneous adhesions from forming.
4-MONTH CHECK-UP :
At this appointment, Dr Lévy will check the range of motion in all sectors of mobility. It should have increased since the last appointment. By this point, you will usually be able to raise your shoulder between 90–120°. The scars should be soft and you can finally sleep on this side. He will prescribe you further physiotherapy to strengthen the muscles and continue improving your passive range of motion. You will also be shown some exercises that you can do at home every day to stretch the joint.
6-MONTH CHECK-UP :
By now the shoulder should be supple and pain-free. The shoulder may not have regained full strength, which can be very hard to achieve. The surgery does not restore the muscles but allows you to use your shoulder in day-to-day life without having to think about it. Patients experience greatly varying outcomes in terms of strength. It all depends on the condition of the muscle before the surgery. This is why it is important not to delay the treatment.
Recovery period & Return to work
The length of time you need to take off work will depend on your job and how you travel to get there. You will not be able to drive for at least 45 days due to the need to immobilise the shoulder for 30 days. There is no reason why you cannot use public transport after a few days.
You can return to work fairly soon, as long as you can do your job whilst wearing a sling.
You may have to wait several months before resuming any manual labour.
If your job involves heavy labour it is unlikely that you will be able to do the same tasks as before, but will have to be reassigned to other duties. The surgery does not in fact give you a “new shoulder”, but a “repaired shoulder”, so you should not subject it to the same heavy loads that caused the first tear.
Potential complications
A wide range of complications can occur with surgery. Fortunately, they are very rare and the various appointments before and after the surgery are designed to avoid them or detect them early if they do appear.
As well as the risks common to all types of surgery and the risks of the anaesthesia, there are some specific risks associated with this procedure.
The following complications may occur with surgery to repair a torn rotator cuff :
SURGICAL WOUND INFECTION :
Despite all the precautions taken by the operating team, bacteria may still enter the wound either during the surgery or afterwards, before it is fully healed. Signs and symptoms of an infection are compromised healing with severe pain, more redness around the wound than normal, a purulent discharge and a persistent fever.
You must tell the surgeon if you see any of these signs and seek emergency treatment.
COMPLEX REGIONAL PAIN SYNDROME :
Complex Regional Pain Syndrome, also known as algodystrophy, is a condition involving pain and other symptoms usually in a limb following trauma or surgery, even if only minor. The syndrome may have a neurological cause such as damage to the peripheral nervous system, affecting either the small fibres which protect from pain or heat stimuli, and/or the large fibres which detect tactile stimuli. It causes pain and severe stiffness that can last for up to 18 months. Patients always recover fully. Dr Lévy will diagnose the condition using scintigraphy (a scan) and will support you throughout, in order to treat the painful and unpleasant symptoms.
MIGRATION OF AN ANCHOR :
This is a rare occurrence that affects mainly patients with osteoporosis or if they try to resume active movements within the first month, despite being told to limit themselves to passive movements. The anchors used to reattach the tendons to the bone can fall off and migrate into the shoulder. A further operation is then needed to reinsert the tendons with a new implant.
RE-TEAR :
The repair should last, but occasionally the tendons can tear again. In most cases, the second tear is much smaller than the first one and usually not painful. Occasionally, the pain returns and the shoulder has to be repaired again. A re-tear may happen after a new trauma or through over-using the shoulder despite the pain.
This list does not cover all the possible risks.
Ask Dr Lévy if you want more information, especially if you have any questions about your particular situation and the advantages, disadvantages and risk/benefit ratio of each procedure.